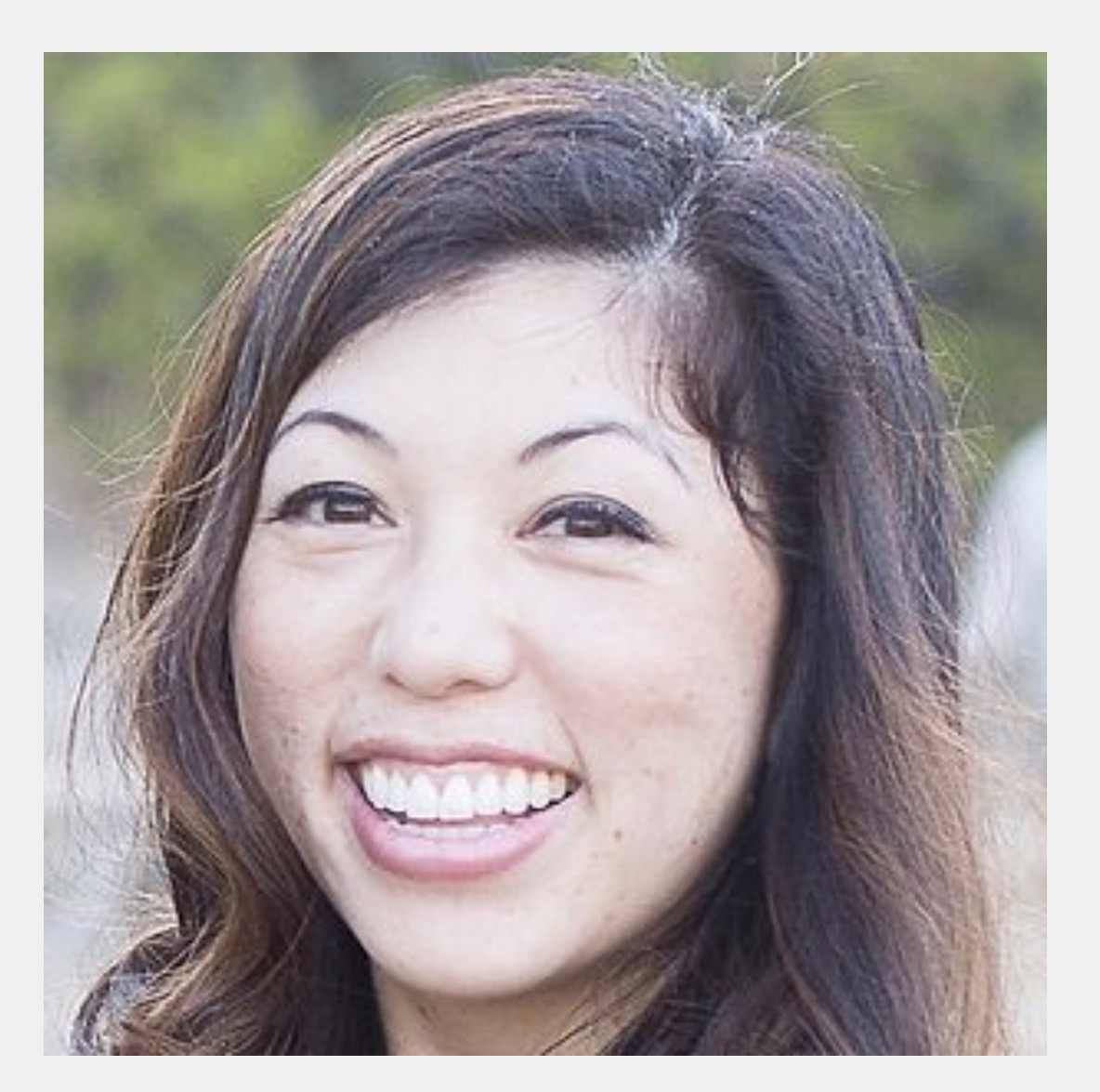
Episode 99: Dr. Lisa Davidson (She/Her) of Insight Primary Care - Denver, CO
- Maryal Concepcion
- Sep 18, 2022
- 39 min read
Direct Primary Care Doctor

Dr. Lisa Davidson has been practicing Family Medicine in Denver since 1997.
She completed her residency at the University of Colorado Family Medicine Residency at Rose Hospital. Dr. Davidson serves as an Assistant Clinical Professor at the University of CO Denver School of Medicine.
She is a huge advocate for the Direct Primary Care movement. After running a traditional practice for eight years, she made the leap to open Insight Primary Care, a DPC in Denver, Colorado in 2012.
She speaks nationally on direct care and enjoys mentoring other doctors who are interested in converting to the DPC model. In her spare time, Dr. Davidson enjoys travel and is always seeking new adventures with her husband and two children.
LINKS/RECOMMENDED RESOURCES:
Doctors featured on My DPC Story as mentioned by Dr. Davidson (click below to check out their episodes):
EPISODE 18: Garrison Bliss
EPISODE 71: Erika Bliss
EPISODE 14: Amber Beckenhauer
EPISODE 61: Delicia Haynes
PISODE 33: Vance Lassey
CONTACT:
Website: Insight Primary Care
SOCIALS:
Listen to the Episode Here:
DON'T MISS AN EPISODE!
SUBSCRIBE TODAY!
Leave us a review in Apple Podcasts and Spotify to help others discover the pod so they can also listen to all the DPC stories so far!
-------------------------
TRANSCRIPT*
Welcome to the podcast Dr. Davidson
in the on phone, but I'm also looking at in the, on
is legit. What happens when I've been podcasting for. You know, over a year on zoom, and then now I'm not sure how to do this, in real lifetime. So yes, it's, it's interesting to see you and see you in two different places.
And this is crazy, cuz it's in your, in your place of, of work where your DPC is in Denver. And it's so exciting because you and I met back in 2019 at the hint summit in San Francisco. And I literally have, you know, just loved your journey because you are a mom and you are doing DPC when you want to do DPC.
And that is not a full-time job. So I love, love, love that. So thank you so much for coming
on. I have to tell you not like I'm I know it sounds like I'm complimenting the host, but I am, because I remember when I met you, I was, I could meet people and within two minutes, like say yeah, they'll do well or very no, or very few people.
Amber is one also. And so as Bree is, they're gonna take this thing so far. I can't even believe it. And like, she's just this like smiley little, like 2000, 19 girl, and now look at you. Okay. Anyway, that was, I had to say that ,
you're so sweet. You're so sweet, but you know,, it's amazing to see.
You speaking in the, at the first tent summit, uh, years ago, and to see where this movement has gone, it's incredible. And you're a Testament to how, when we work together and we, help each other along the way, how we can make this movement really different than anything we've ever seen before.
So it's awesome. So, I wanna start with that. You've spoken about, taking the leap into DPC, but I wanna actually just point out that you have taken the leap twice. You went from residency into an employed position, and then you left your employed position to open up your own private practice.
So how did you even have the courage to make that first jump going into a private practice when you know, the, the trend at the time that you left, your employed position was to be
employed? Exactly. I remember a couple things from my residency director who was very wise and he said, when you guys graduate, you're probably gonna stay at your first job for a couple years and then you're gonna go somewhere else. And I had accepted a job with these amazing women out of residency. And I thought like, that's stupid.
Why would he say that? I love these women. I'm gonna work with him forever. And so. Um, I went to work with them and I lasted about four years, so twice as long. And, but at year three they were barely making it and they were private practice. But I . Was looking at it and I'm like, these women are amazing doctors, but they don't know about business.
And so I don't feel like they're ever gonna survive. Like they're, wonderful women, but how are you not making enough money to survive? And of course it was also part of those times in the industry and people were getting bought up. So I was naive or stupid or crazy. And I just said, I think I can do this better.
So I'm just gonna for fun. Try. Why not? So, I worked for like a year researching how to do it and I didn't wanna have an office manager. I just wanted do it myself. And so, um, my dad was an accounting teacher and an account. So I thought, well, I must have some genes for accounting, so, so let me, I think I can do math.
So let me just try to get my insurance contracts. I had a wonderful biller. I had an amazing PA who I still have. I had an amazing nurse. , I had an amazing front desk person. So I thought, well, let's, let's go, let's do it. Let's bring some of these people over. And the front desk didn't come, which was sad, cuz I, I loved her, but I, uh, that was one of my fun staffing issues for the first few years in fee for service practice.
But we found a space and my husband is an awesome architect and he built out the space for me and we just opened and, and uh, it happened .
that's incredible. And, you know, especially for those people who are thinking of opening after residency, there are people out there who are considering, well, maybe I'll open fee for service first and then, you know, potentially move into DPC.
So if you had the choice, would you have chosen to do DPC given that at the time it was still such a new, you know, it's not a new model, but it was a new model.
Yeah. So would I have done it differently back then? Like no way, because it was back then, would I do it now? Fresh outta residency? Ah, I love the people that do, and I think you're all amazing. Would I have had the courage? I don't think I would've had the courage that you guys had only from the clinical aspect, because I feel like I, I needed to see like, you know, 20 patients a day for a few years, but we have so much support now in the DPC community that I think it makes sense to go straight outta residency and do DPC now because we have that support in 2008 or four.
No, no way, but now, yeah, I probably
would've. It's so good to hear somebody who has been in practice for so many years, really be able to reflect on both of those times, like the time we're in now. And then the time that you left your fee for service job, , as an employed physician to open fee for service back when you did.
So now when you were talking about the insurance contracts and whatnot, and you were realizing that the business of medicine really matters when you're in private practice, whether you're in DPC or fee for service, how did you really, start to understand your business when you were in fee for service to make your office efficient and profitable.
The secret for everybody in DPC, anywhere, anywhere you surround yourself with people who know what they're doing.
Like I had a really good CPA. My biller was phenomenal. Like I couldn't have done it if I thought I was smart enough to do it all by myself back then. And so I respect people who know what they're doing and in family medicine, we're good at that. Cuz we respect our specialists cuz they know more than we do about certain things.
So I listened to them and I learned from them and sadly like we were very popular practice. We were busy, but it was, I didn't pay myself like a lot of the time I just skipped my paycheck. And I would, it was the classic story of a new mom sitting on the couch with the baby next to him, you know, doing my charting at nine o'clock at night.
So it was, it was profitable to a point. I don't think I broke six figures while I was in private practice for eight years, trying to make it work with insurance. And I worked three times as hard as I do now.
It's so ironic, but it's so insightful to hear you say these things because you've really lived, you know, a, a decent time in fee for service as well as now in DPC. So I wanna ask about your, your courage and your jump to leave your fee for service, private practice, to go into your own DPC.
How was the courage and that jump different than when you had made the jump into your own private practice previously? Oh, that's a good
question. I was 12 years in fee for service. Totally exhausted. Two little kids, um, a fantastic husband who was so patient with me working to the bone, not making enough to pay off my student loans.
And, , so I was either gonna like quit medicine or go work at Kaiser and be miserable or, I don't know. So I was like, there has to be something else. , so I was out of desperation. , and then, my dad had died in 2009 and that made me start thinking about the world. And then my mom passed away in 2012.
And that, that those both just woke me up because they saved, they had four kids, they saved for their whole lives. To put us through school to make sure we're successful. They always put off their life. They're like, we'll do it later. We'll do it later. We'll do it later. So they both died, like barely being able to travel the world.
Like they wanted to, like, that was always their dream. Um, and so I thought like, I'm not going, I'm not gonna do that. I'm not gonna honor them by working myself to the bone, my whole life and then saving and saving and saving and then dying. Like, that's not how I'm gonna honor my parents. The passion behind my change was what gave me the courage to do it.
And everybody in DPC has a passion story. I bet you,
I would definitely agree with that for sure. And, you know, it's, it's so funny. I remember, , that the person who had told me about DPC was actually , Dr. Ariana DERs, she's an orthopedic surgeon, but I remember she posted one day, I think, on the DPC docs page. What was your, uh, last straw?
And it was like, well, there goes the. Kerosene on the fire and then you had 127 posts within, a few hours because that's how everybody has had their, their passion come from a particular spot, whether that's because of, not being valued in the system, whether it's, they are valuing themselves, whatever it is.
And I love that your, your honoring your parents is a part of your story. I think that's so awesome. Yeah.
And I love, that's the part I love about hearing like you and I just were exchanging stories of how we met my, our husbands, but like hearing people's what was your passion moment? And everyone has one.
It's so good. It's so good. So now when you took this, this passion and you wanted to mold it into something that possibly was medicine versus leaving medicine, you had mentioned that you learned about Pam wel as well as, , reading Dave Chase's articles and, , Pam wel, for those of you who are not familiar is, , the creator of the ideal medical practice or imp.
And then, uh, Dave chase is one of the co-founders of health Rosetta. And so when you were reading and learning from those two individuals in particular, how did you start thinking about your DPC, , in terms of, \ , did you start dreaming or actively planning or both at that time?
What a great question.
Um, so I think of Pam as the heart and Dave as the brain. In my DPC baby. So Pam inspired like that hard in me and, looking at ideal medical practice and I was like, that's amazing. I love it. The connection with your patients, blah, blah, blah. And then I, and then Dave, I was like, okay, but what about the nuts and bolts?
And so Dave was like, I read this really, really old article from a long time ago. And he, and he used like, what is that? I love that phrase, innovative disruptor.
So it like stuck with me and then, and Pam too. And then this, this popped into my. Idea popped to my is like, I need to shrink in order to grow. And I think I meant I need to shrink my practice in order to grow as a physician. And so I used both like the heart and the brain of, of the DPC ideals back then, along with Garrison and Erica and, blended those together.
So I woke up at four in the morning, one night and went to my kitchen table and then I started the planning part.
And when you were, going forward and learning more about DPC and you were finding individuals that were were actively doing this, this idea of direct primary care and live time in addition to, you know, Alliance in addition to, what Dave chase was talking about.
You had found people like Ryan, new HLE and Sharon, George, when you were planning, when you, when you said, , you whipped at that paper four. In the morning and you started planning how did that change your, plan or your ideal practice for your future?
Oh, that's a great question. Um, yeah, I liked the, I idea the ideal medical practice idea, but I did obviously I'm way too social to be working like alone in a clinic. So I like, I need to love my staff. I don't wanna be alone.
And then I think I found Ryan and I was, I called Ryan and was like, What are you doing? And he's this young guy and he is telling me all about it. And he was, I thought he was really brilliant. And I, it was so funny cuz you could call and like Sharon, you can call people back then, like the 20 people that you could find on Google that were doing it and talk to them all.
And one of the things that struck me today, um, I was reviewing like who all you've interviewed in your podcast? And I was like, oh yeah, I know that name. I know that name. I know that name. And then there were like a ton more I'm like, I don't know that person. I don't know who that person is. And I thought this is amazing.
Like I dunno, most of the people in DPC, which is that's great. Like that means it's too big to know everybody. It's so exciting.
When you talk about calling people, like calling Ryan and calling Sharon, Sharon was in practice in Irvine at Renaissance DPC. She had, you know, a micropractice in terms of she was doing it out of her home, like Neil Douglas style nowadays. And so when you saw that, like what, what did you pull from her practice similar to how you did when you were talking with Ryan that you built or did not build into your practice at insight?
I dunno if it was specifics the way I built, but it was just like the feeling of who they were and their personalities, and they were very, um, they could draw you in very naturally and they were very comfortable to talk to and they were comfortable with their model and they recognize that.
Really, really brave. And, and they were pioneers and they were, the bravery in them is what just sort of struck me. And I think that today, that's why people always say go to DPC summits in person because we always joke that it's like a cult, but it is because the energy that our is at those meetings is ridiculous.
And it gives you the bravery that you need to do it. Like it really does still.
So now I wanna ask something that is very different for you because you were going from your own practice into your own DPC.
What were some of the things that you realized that you did not need that you may have needed in fee for service, but not for DPC?
Oh, the hardest one was, I didn't need my biller anymore and I absolutely loved her. And so I was trying to figure out a way to bring her with me. And there was just no feasible way.
And she was such a good biller. Um, so I didn't need her and it was broke my heart. Um, my, I had an RN that I worked with for like 12 years who was also phenomenal. And she came over with us. And then after a little while we both realized like she wasn't being challenged and she wasn't being used in the way she could be.
Cuz she was so good. And so we both realized like she was like, I need to move on. And she did and we're still friends, but I really, I missed those two people. but you don't need 12 staff. You don't need six phone lines, you know, there's so much crap that you could trim off your overhead. That's absolutely amazing.
You can get your malpractice at like a fraction of the cost. Well, I am, but I'm also part-time.
And I think that when we actually look at what do we need to function, what do we need on opening day? I mean you see people who are doing , telemedicine only then doing in person visits later, you see people who are doing, a lot less urgent care shifts or whatever because their overhead.
Is not going to need to cover certain things like you're mentioning. Now, when you look at, when you opened your DPC, what are some of the things that you needed that you didn't have in fee for service that you needed to, to make your DPC function the way you wanted it to?
I'm gonna answer all the questions differently than you think I'm gonna answer them.
You need boundaries. I needed boundaries because you're, you're so like, I want people to join. I'll do anything. I'm desperate. Like I'll come to your house at four in the morning, you know? So what do I always say? You under promise and overdeliver, you don't offer like I'm up Saturdays and Sundays.
You're committed forever. So under promise over deliver. So boundaries with patience, I will always push that DOE and I are both the same way with that.
It's so good though. And it's really something that when you realize that, you know, if you're doing DPC, this is your practice. And so you get to, you get to call those shots. That's why, like, one of my favorite visual representations of DPC is, you know, the sticker on the front door that says hours by appointment. Only's the best. Yes, exactly. Now you mentioned that you're a part-time DPC.
So what does that mean in terms of what's your day to day? What, days of the week do you choose to work with your patients?
Oh, okay. So I'm in the office seeing patients, um, Monday, Tuesday, Thursday, and Friday mornings. and then Wednesdays I'm totally off and Friday afternoons I'm off and then. In the afternoons we're doing mostly telehealth.
especially since COVID, it seems to work really well. So we, we work smart, not hard. We pack our mornings in pack, meaning, you know, like six people. But, um, we do it that way. So, um, I can be home a lot. And in the beginning when I was going part-time I felt like super guilty, cuz I wasn't working a
hundred hours a week.
I was like, I should be working more. And my husband was
like, but why? Like you've worked so hard and you're doing a good job. So why I'm like, because, so I finally learned to let that go and I gotta give a shout out to Amy Walsh because one day when I saw at a meeting or something, she was like, dude, what do I, how well, how are you doing this?
What do I do? And now Amy Walsh spends like her summers at her lake house, like a lot. So
she's doing it too. And I'm so
proud of her. That's great.
It's interesting that, you know, when your husband is saying, why like in your brain and in your training, you, done over 12 years of, of that.
And then like to change that habit, I would have it changing as hard. We all know that, but especially when professionally, we only really know one way leaving residency and, and the fee for service world that we're trained in. So it is really challenging, especially when we're, realizing that we might be getting into fee-for-service type habits again, and then we realize we don't have to.
So when you talk about, you know, mentoring and talking with each other, it's, it's, it is so important because we all, I feel have that shared, you know, oh, these are the bad habits that we were that were instilled in us when we yeah. When we trained. Yeah, totally. And,
um, and I'm gonna, I have to put a qualifier in here, like.
I think about you. And I think about Vance and you guys are all in and you you're bad asses and you do everything. And so I have to say to all these people, all these listeners, um, I live in Denver. I live in this city. I know a ton of specialists. We have 24 hour, like everything can be gotten in this city without me.
So I know that, um, my patients are well cared for, even if I'm not around they're well cared for, because I also, cuz I have a PA um, I live in a big city, so not everybody can do part-time and not everybody can do this practice and not everybody wants to do this practice. So I'm only speaking to the, like those
people.
Cause I don't know that big trees you could actually do. Part-time I, maybe you can. Yeah. I mean, I probably could, it just be different than
Denver. Yeah. And that's the thing, you know, it's, it's like, like Garrison list says, if you've seen one DVC, you've seen one DVC. And so, yeah, I think that especially the, the finding somebody who , you can relate to whose schedule you wanna emulate or whose ideal practice is exactly what you are wanting to build or whose actual practice is what you're wanting to build towards, keeping in contact with those people can really make a difference in terms of building out and sticking to your, your plan, your business plan, your dream plan, whatever it it is.
And would say it also depends on, how financially you might have set up your business model too. , those are things to look at. You know, if you wanna build a practice, a particular way, just like how you did, how you talked about how Pam w was the heart and Dave Chase's words where the brain it's like, you have your financial part of your DBC, you have your, relationship based practice and so finding a place where they work together to still work towards your dream, it absolutely is possible.
Amen's sister . Yeah.
Awesome. So now, who was with you staff wise on opening day?
Oh yeah. So. Um, I had, Melissa is my PA and we've, I got married to my husband in March of 2000. And then I started working with Melissa and fee for service in September of 2000. So we've been like work married to each other for as long as we've been married to our husband. So, so she was with me and, I had a, a person who did front desk, her name's Chelsea. But her husband was stationed first in San Diego and then in Hawaii. So she was like my virtual front desk person. Chris, my front desk from my fee for service also came over with us. She had joined in 2011, our staff. And so she'd only been there like a year when I, when I made the jump to DPC.
So she was very brave and trusting to do so. And then, my nurse,
and when you were transitioning over from fee service to a completely different pace structure model, how did you set your pricing?
Oh, so that was, it started at the four in the morning kitchen table. And I was just throwing out random numbers on a paper. And then it ended in a California pizza kitchen with my husband on a napkin . So like Ryan new hopeful, like he was in a college town and, and I, his prices back then were so low and I was like, honey, I think these prices are like too low.
And so we set 'em higher. And then Ryan, wasn't growing very fast in the beginning. I'm gonna out his story. And, um, so then he was like, he raised his prices and like suddenly he grew like wildfire. So it's like, there's such a thing it's not charging enough. And people thinking like, well, I, why is this so cheap?
Like who is this person? You know? So that's how my fee started and randomly on a napkin.
That is awesome. I hope you framed that because I totally have. Santa Cruz DPC brochure that I didn't have any. So I didn't have any scratch paper when I was talking to Dr. Janine rods out in Santa Cruz at Santa Cruz DPC. And so she handed me a brochure from her clinic and I still have it to this day.
And I was like, oh, this is where she told me to, you know, talk to James and Emily at, at, um, calcium and yeah. So I totally like those. Those are like my, my mementos of like, remember when, like this was, remember when you were so excited and, and you learned about this. So yeah, I, I hope you frame that.
Um, I love cause those are, yeah, those are like, your beautiful brain, our, all of our beautiful brains able to just be free and to be able to plan and dream, um, in the manifestation of, you know, writing on napkins or whatever it is. So that's awesome.
Um, we put 'em in the DPC museum somewhere.
That's amazing. Oh man. So when you were, um, after you had had staff join you, and then you set your pricing and you opened, how did you train your staff? Because yes, you guys had worked together, but now you're working together under the, the umbrella of DPC. So talking to the patients is different. Having them understand the model, as well as them being able to explain the model to potential patients joining your practice, how did you train your staff and train , the clinic to have a culture that favored DPC.
Oh my gosh. Yeah, we had, it was like speaking a new language and so we had to what helped cause back then nobody knew what it was. So what helped is we had these, almost like seminars for our existing patients who were in fee for service to come and learn about DPC. And so that's how I kind of perfected my communication of what it was. I would tell them.
And then, um, slowly but surely like our staff, they would also like learn the language of DPC and learn what to say and how to say it. And so we all learned like the six months before we were gonna make the jump to teach the patients, we learned the language. And so my staff's amazing. They were all in from the beginning.
And so when we opened, they sell the model. They Chris and Chelsea, they know they're the, they work at the front desk, they do the blood draws, they do the labs, they do the triage. Like they know how to sell it just because, um, of the way they learned how to speak it. So you have to learn how to speak it first. So it was so fun cuz we were learning together and it was, we were really busy, but it was all like a different energy.
We were excited. We were busy in a different way. We were busy like growing and marketing and uh, you know, learning how to do things like by the seat of our pants and it was so much fun.
, when you were talking to your patients in person, when they, when you had those, you know, seminar, meetings, did you find any other marketing strategies that worked and did patients really understand DPC because they already had you as their doctor and they understood the value proposition of maintaining that relationship?
Or did they really not get DPC?
Oh my gosh. And I'm sure everybody goes through this still to this day, but they did not get it. They didn't get it. Um, like I would explain it and they would, they would just come back to me and go, but I have insurance, like I know I just explained how it works with insurance.
and then. We had one of the meetings. We had this really funny patient. She was there and all these patients were confused and listening. And then I felt like I paid her to, to be there, but I didn't like she was a plant cuz she was like, so what you're seeing is for the price of like a nice dinner for my husband and me a month, we can get all excess medical care I was like, yes, that's exactly what I'm saying.
So no, it was like pulling teeth and I always, I like to call it like the lean back, sit straight, lean forward, because as people start to understand it and that goes for not just patients, but like anyone you talk to about it, like specialists, administrators at the hospital, they're leaning back in their chair and they're like skeptical and their arms are crossed.
They'll have their hands crossed, like, and then it'll be leaning back in their chair and then they kind of start understanding. So they sit, sit up straight and by the end they're like leaning forward towards you. Like tell me more. It was so funny. I, it happened all the time. Does that ever to you, have you paid
attention to that?
So it's funny because I would do. Initial meet and greats on zoom. And so it would be so interesting because one, doing zoom was actually a screener for me to be like, how is tech for you as a patient? Because , my practice is definitely like maximizing tech.
And then seeing a patient in person if needed. And so I would say a quarter of the time, the people I was doing meet and greets would have a black screen because they weren't necessarily using zoom with the video on or whatever the issue was. Yeah. And then in terms of, I had been really surprised.
Some people, they just understood that. In our area where there's very little access to care. They're like, whatever it is, I can't lose you as my doctor. And then I had other patients who were like, yes, the, the, I love that analogy of the like crossing the arms, lean in, lean out, lean in, and the like going back and forth because I remember some of the conversations, my previous patients from my former, fee for service practice, they said those words, but I have insurance.
And ironically, , maybe a couple of weeks ago I had a patient who's been with me since early on. Ask me in a portal message. Can you just fill my insurance? How come I'm paying out of pocket. So that, that, culture in us to use our, you know, as Jeff gold puts it to swipe our, our insurance cards, like credit cards is really, really ingrained.
Because you know, patients sometimes forget that they have access to us, through whatever means they do, patients see their loved ones using their insurance cards. And then they forget that like, oh yeah, I'm actually doing this separate model. So I see the gamut of, differences in getting it so to speak, getting the DPC model what you're saying. I can totally relate to it. So, yeah. , that's so funny.
I was so overconfident that everybody would understand it. And like there would, they'd be beating down our door and I quickly learned that wasn't the case. Cause I think we have, like, I don't know, I don't even remember some number of thousands of patients.
And I was like, oh my God, we're gonna be full right away. And then we only had like 200 people join right off the bat. So then once we opened, I did marketing and I like, I did sports physicals for the local high school. And we had like ads in the newspaper. We, we weren't doing, we were doing Facebook a little bit, but you know, mind you, this was 2012.
So we were doing some old school stuff. so we didn't have to do too much marketing cuz word of mouth just took off PR and our, our little neighborhood didn't have a ton of primary cares. So it was, it was pretty easy thankfully
let me ask you here. The 200 patients who joined, which is. Amazing. Like, even though, you know, it's a small portion, it definitely allows you to have a member base, to have the, income coming in.
But I wanna ask who were the patients who found the value proposition of having you as a doctor having, you know, the, the DPC as a model who were the people who valued that and joined your practice and have most of those people stayed today?
Okay. So that's so interesting. Cause I was thinking about it and yes, the early adopters are still with me now.
Like it's so crazy. So many of them, so they've been my patients now for like 20 years. I mean, it's like I have, I have a couple patients that I took care of in residency clinic and they're still my patients. one of them. Moved to the south and my heart is broken and I'm definitely gonna go, gonna go visit her.
But, um, a lot of them, yes are still with me. their family has come and joined, you know, like, like their brothers or sisters or husbands or whatever. and one of the, I think it was the first person that signed up, like physically signed up. It was like a year went by in DPC in 2012. And I hadn't, he hadn't come in a single time.
So I think I called him and I was like, Hey buddy, like you were the first person to join my new practice, but you haven't even come in for like a physical, like, do you not wanna like, spend some time with me since you're paying me? And it was so funny cuz he was like, I dunno, maybe 40. And he said, um, I don't need anything right now, but I know I will at some point.
So when I need you, I need you. And I was like, oh, okay. Um, so then. Fast forward to like two years ago. Um, and he gets prostate cancer and he's doing great, but it's so funny because he remembered that conversation that he and I had, you know, 10 years ago, he said, remember when you called me, cuz I wasn't using you.
And he said, I told you this would happen. And I was just like, oh my God, mind blown. I love it. It's it was so funny. So I just, yeah, it's amazing who joins and who doesn't join and then who didn't join initially, but then six months later, you know, calls saying, please can I join? Because I realized what care there is out there in fee for service.
Oh man. So that
was pretty fun. Yeah. And how, how relieved I'm assuming he must have been to not have to question. Well, how long does it take for me to get into my doctor? To discuss this because, we've all seen so much piecemeal care, especially when it comes to really, you know, concerning diagnoses like that.
You know, cancerous type diagnoses where, yeah, I got diagnosed with this on my mammogram and it's gonna take, you know, how many weeks to get into, see, you know, X, Y, Z. And we have the ability as relationship based doctors to, okay. I get that. You can't see potentially your, fee for service.
Doctor, but I can call on your behalf to talk to, an oncologist in that cancer example, um, to start getting, you know, your work up going or images ordered, figure out, can we, you know, do a cash pay order for this image that you might need rather than waiting for your insurance to cover it, whatever it is so that your care is not delayed, any more than it needs to be because of the fee for service model.
So I think that is awesome. And I'm sure that there are multiple patients out there who can relate to that experience of, yeah. When I need my doctor, I actually do need my doctor. And that's what DPC is built perfectly for. Oh
my God. Yes, exactly. It's all about the relationship and another perfect example of that is I love meeting specialists, so.
Because, you know, I'm social and all, I like to go out and have like a cocktail with a specialist or something , , or a coffee. So I, I met serendipitously, I met a breast specialist. Who's new to my area, um, earlier in the spring. And we got along great. And nowadays it's so great cuz we have everybody's cell phones.
And so literally like two weeks after I met her, um, one of my patients was, came back with a SU suspicious mammogram. They did the biopsy, it was malignant. So I texted her, this breast specialist. I just met, she got her this patient in the next day and did her surgery the day after that. So it was literally two days from her biopsy result until she had her surgery.
And if I didn't have that relationship, like she wouldn't have gotten that. And if she was in fee for service, she wouldn't have gotten that. So I was like, that's amazing. It was two days like, come
on. That's incredible. And, that's why I still call my old attendings from residency because it's like, they know who I am
and so if I'm calling them with like, Hey, I really need this person to get in. I love that. Like you're saying that relationship, they will make changes in their schedules, adjust what they can so that, the patient can get seen. Like that's, you know, it's like I get that DPC is not for everybody.
a Huge this podcast exist is to, to put it out there as an option for people to consider, no matter if you're in fee for service or in DPC, at the core of why we are, physicians goes back to wanting to take care of our
patients, you know, this idea that we take our Hippocratic oath and.
The, the idea of do no harm. We are really looking out for patients at, at the, at this core of everything we do. But when it comes to then taking that desire to help a patient and putting that desire into particular models fee for service of DPC, the outcomes are different. But I will say that when you show as the DPC doctor, especially that, Hey, you're involved in your patient's care.
Even if they're seeing a specialist in fee for service, it really can make a difference in terms of their outcomes. When they see like, oh, like this person isn't just being referred, they actually have a whole story and a whole support system medically behind them. It makes even specialists think about care differently.
And so I've seen mountains move just like your patient with the breast surgeon. I've seen those examples happen even more so in DPC because we have the time as physicians to then call the specialists and connect with them and say, Hey, this is exactly why I'm needing, this patient to get care sooner than later.
So I absolutely love that. Exactly.
I love it. And oh, I have to tell you a flip of something that caught me by surprise. I was doing a talk the other day at one of the hospitals here to like the me medical executive staff. And I was talking about DPC as a model. And one of the specialists like raised their hand during the talk and was like, well, your patients are sort of being groomed to expect a higher level of care so that when we, they get to us and we're busy, we can't really give them that level of care that they have been taught to expect from you.
And she said that, and I was like, did you hear what you just said? And. I don't know how many people listen to this. Maybe I don't, she was an oncologist so I was like, oh my God, like you just said that, and you're an oncologist and you're worried that I'm spending too much time and giving too good of care to my patients.
That's what you just said. And , I was very gracious about it, but I was turning out in my head on the way home. And I was like, I can't believe that that just like she was judging me for taking good care of my patients and spending time with them.
wow. Yeah. That's that is an absolute opposite example of relationship based care. So, and it's, it's scary because especially, , dealing with a diagnosis of cancer or, end of life type of diagnosis to have the support is insanely important, at that time, especially. So with your practice being so successful and , how you mentioned the original patients who joined a lot of them are still with you.
How has churn been for your practice over time? Because, I think about what are the reasons that patients have left? Like you said, your sweet patient moved to the south. What are the other reasons that you see people churning in your DPC?
Most of them are that they move, the other ones, a little bit during COVID, because we had enforced CDC recommendations, some of them got frustrated and didn't agree.
So they chose to leave. I have some other patients that, I, I really somebody who likes to empower patients and, and make sure that they take accountability. So if they're asking me like to fill out F M L a. They hate their job. And they tell me, I hate my job. Will you give me F, M L a, like, I'm gonna be really honest with them and say, I'm not gonna do that.
It's how is that gonna help you advance in your life? If I bail you out and give you a parachute, just because you don't like your job, what, what do you think you should do instead? Why should probably find another job, but, and I'm like, I'm not going to there's no, but here. So I'm pretty strict on that stuff.
And if people don't like that, then either I, I tell them that it's not an optimal relationship or they choose to find somebody different. And so that's part of shaping your practice and you all need to swallow your pride. If somebody quits your practice for, because they don't like your shirt, it doesn't matter.
Like don't dwell on it. Don't take it outta the insult. Don't be pissed off like it. Let them go. It's okay. And you're gonna shape your practice and draw in the patients that you draw in the patient's. With the energy that you give. So if you hate your practice or you hate your patients, look at what you're doing and what you're putting out there, because it's not the patient it's usually you and what you're doing.
Hard
truth. There.
Yes, if you're feeling stressed and your patients are giving you that feedback or that, that there's not a, a good fit for patients who are joining stop and reflect on what is the situation going on
and now on your website, you have our practice and wait list are full. And when you try to click on the button, it doesn't click anywhere. Do you still have people contacting you? And what do you do with those people? do you, you know, say, Hey, here's a list of DPCC doctors in the Denver area. How do you handle contacts who might be interested in DPC, but are not going to be a good fit for your practice?
Yeah, that's a tough one. It's so funny also because we started our wait list a long time ago.
And as soon as we went on wait list, and I think a lot of people across the country realize this when you have a wait list, suddenly it's like, you're the Ivy restaurant in Beverly Hills. Like everybody wants to be in your practice now because you're a wait list. So it's, it's funny from a marketing perspective.
even if you're not full, you might try and put a wait list on your website and see what happens. But now we're like very our wait list. Is it? It was, I don't know. It was like approaching 200. It was just bad. So we were like, we, we can't. So we turned it off. So it's really hard because everybody will like, oh, I've been your patient for 20 years.
Or a doctor will call and say, oh, will you please take my friend? Or, you know, like do me this favor. Um, and it's easy to try and play favorites, but it's, it's really not fair. So I tell people like, I am like the most diplomatic person I I'm sticking to my wait list. I can't. I can't play like favorites. Um, so I just have to be really clear with that and it's frustrating, but we do have amazing DPC doctors around town.
so we have the ability in Denver, thank God to refer to each other. However, they're all getting full too. So if anyone wants to open up a DPC in Denver, come on out, cuz we have plenty of patients to go around
and plenty of support, you know, in terms of, we'll get into how you're able to continue living life, the way you want to, after you open your DPC, like taking trips when you need to taking time for, you know, yourself whenever you need to.
If you guys have new features coming down the pipeline or whatnot, , as they're, you know, sitting on this potentially perpetual wait list,
You're totally pinning me down. because we haven't like we haven't been reaching out to them and, um, oftentimes they'll reach out to us and say like, am I moving on the wait list?
And, and we're always, our staff is so nice and we're always like, you know, you're, you're here or what, whatever number you are. And we're really sorry. It's still, you know, it was such a long wait list,
the reason I ask that too, is especially , the part about referring the other DPCs is that Dr. Eric, a young, , in white marsh island, Georgia, she had said, you know, I'm full, but there's a pediatrics DPC right across parking lot from me, you know, you know, you can go there wherever.
But I think that, , if a DPC is similar to you and that there are other DPCs, open opening, and you guys are geographically close or whatnot, collaboration in terms of, Hey, I'm not accepting, but here's the link to, you know, um, Johnny apple, C DPC or whatever it is, and they're accepting patients.
That's one strategy that could be used to collaborate within a community. So that more patients are coming over to DPC, um, and that word of mouth is spreading for the whole community. So just one, one way, the one thing that I think about when I, , hear what you say, and then also think about what, Dr.
Young is doing down in Georgia,
but yeah, and that's a great idea on my website. I can put links to my colleagues. You are right. Totally gonna do that.
Yeah, absolutely. And that's, and that, that goes back to why I love DIY websites because you can just change those links anytime you want. So that's amazing.
Yeah. Yeah. So since being, since being a DPC doctor, I wanna ask about, your coverage for your practice, because you've been able to go to New Zealand and do some Bunge jumping, and you've been, you've been traveling as you wish to travel.
And like you, you talked about your parents as you wish to live your life because of what you learned from their experience. But how are you doing it when you need coverage? Whether a person need, whether a patient needs to be seen in person, or if a virtual visit is okay to cover their. Yes. It's
actually worked out amazingly well, cuz of Melissa, my PA um, we cover for each other when we're both like when we're on vacation, like she's gonna go to, um, Italy in October.
And so it's, it's easy that way. And then on top of that, I have like Michael Keller and Derek Waban Andre Feld. So the other DPCs in our area, I can just text one of them and say, can you cover if Melissa's not available? And we usually end up. Covering most of their patients through telehealth, you know, we, we cover for each other or they cover my patients through telehealth.
It's worked out very, very well in the last 10 years. Like it's been pretty smooth. Um, and I don't, we don't have any financial arrangements, we just help each other out and it's actually felt normal and great. And it's pretty easy. , like a couple of 'em use elation so they can just send me charts.
Like their staff will be working when they're on vacation. They'll send me charts so I can see their patients if I need to. And I have, a login of my own to elation, but I can have their charts. and then, yeah, so it's like the support staff actually helps make call easier because the support staff in all the offices is still there answering phones.
I always tell my patients when I'm going out of the country. So. the volume of requests definitely goes down while I'm gone. And that helps too, that helps the burden of the practice.
And, to clarify, say somebody's on a different EMR and , you're like, oh, I'm doctoring for this patient over telemedicine, but I'm not sure like your allergies or whatever, are you just relying on the, office stuff to really be able to get you , the paperwork or the history that you might need?
Like they'll fax over whatever you need electronically or something like that, so that you, have, the components to make the medical decisions you need to make at the.
Yeah, this that's what we do with the support staff. They're super helpful. And I'm sure I know the tech savviness of you you'd probably figure out something even better than that.
but thank God for good support staff.
Yes, . It's awesome. And you know, it's something to, to talk about, like, if you are wanting coverage, that is another type of boundary for your practice, but you can absolutely encompass your community in that boundary. So like, for example, in California, we have this DPC, California syndicate, that's our like, you know, DPC, California Alliance type of group.
And, we've been talking about, how do we share calls, , via telemedicine? If needed, if, you know, a family wants to go outta the country or, if a DPC doctor wants to just not have to take calls for whatever reason, how do we set that up?
So, you guys have just worked it out, but thinking about like, are there people that are in your community that are gonna do that? Do you want to figure out some kind of way to make sure that the tech integrates or that the workflow integrates to be able to cover?
how do you, compensate if somebody wants to be paid financially? So thinking about those things to set those boundaries up, to protect your vacation time, or, , time that you might need away in an emergency, those are definitely boundaries. And then, , on the patient side of things, when you talk about boundaries saying something like. When I'm gone care will be exclusively delivered through telemedicine is a way to set up those expectations also because then, you know, a patient knows like, okay, like if I can't, if I have a, , a brown recluse bite or something that I need actual physical care for that, I'm not going to be relying on my doctor, who's in Italy or whatever, I'm gonna go to the urgent care.
So they have that, those expectations built in as well.
Yeah. It's all about planning on the front end. It's it's totally great. And I love that the syndicate is doing, talking about that because Denver we're unique cuz we are just sort of organic. Like we organically did this, with ourselves, but that's not practical for a lot people.
So if you making a plan and making like some sort of contract makes a lot of sense, probably so good job on the syndicate
that? That was Dr. Fiedler's idea, in the bay area. So yeah, definitely. Oh, awesome. Yeah. And in terms of, coverage, you also have, and this is something that I've always found interesting about your website. You also have a link for aftercare hours to particular insurance companies.
So like the nurse on call for blue cross blue shield or whoever the company is. And so can you tell, can you share with the audience, your thoughts in putting those links on your page and how have patients used those resources?
Oh, that's a great question. well, because I'm so old now and I had, I know I practiced like before EMRs and before, like Google was barely a thing, Call used to be really important in primary care when I delivered babies. Yeah. Call was incredibly important. Of course, like you had to be on call all the time, but it's 20, 22.
Like people, people look up more medical crap online than they should be doing. so I figure why don't I give them at least some good links to go by. And then we have this amazing thing called dispatch health in Denver, where they will do house calls. And I think the I'm gonna get in trouble if I quote the flat rate, but I swear if it it's self pay, I swear it's like 250 bucks.
So like that avoids an ER visit. It was incredibly helpful during COVID. they are like our call, like they can take after hours and give after hours home care for our patients. They also do bill insurance where people have insurance. So, people are smart. And if you train 'em to, like I said, be empowered, they can answer a lot of their own questions without having to pay you on call.
And again, I'm in Denver. We have a hospital on every block. We have urgent cares more than we have Starbucks. And so if primary care on call, think of one thing that I could help somebody with after hours in the middle of the city, that they couldn't wait till morning for, or if it's chest pain, why are you calling me and not going straight to the ER anyway, I know some people will totally disagree with me and I know, I see you thinking about trying to think of one that would come up but they can still call me.
I mean, they can still like email my, my portal. Like I love my portal, so
yeah. I love though that you have this idea of empowering your patients and your website reflects that.
So one of my patients, like this was quite a while ago when we first started DBC, , she paged me at like 1:00 AM on a Saturday because she needed her estrogen refill.
And it's cuz she's a nurse at the VA and she works nights. So she was like, well, I'm awake. I'm just gonna, you know, like, but she paged me. I called her the next day. I'm like, dude, what are you doing? Like, why didn't you, you woke me up and she's like, oh my God, I'm so sorry. I know why I did that. I was awake and I, and so then we're fine.
Like I called her out and we laughed and we're fine. And she hasn't done that ever again. So like, come on, you know, but if you have 3000 patients, you can't say, dude, what are you thinking?
Not at all. And, and with 3000 patients or more, especially in beaver service, it's really, I mean, they, they would hardly even get to talk to you because it's usually like the layers of admin before they even get to talk with you.
So, yeah. , that's cool though, that you were able to, to do that, and just reset the expectations and those boundaries, on a personalized level. Now in terms of other features of your practice, you offer immigration physicals. And so can you share about how you got involved in that and how that works into your practice?
separate from your regular DPC members?
Yeah, it's actually really cool. We've been doing those for, I don't know, 20 years. So people to immigrate to Canada, Australia, New Zealand have to have this panel physician's office, do their immigration physical and it's, it is like silly paperwork. to move to those countries.
And so my PA has been like the expert of doing those for well, since, yeah, since I graduated residency, so we were doing 'em at the old practice and they just moved with us, these immigration physicals. And so, it's a cash based, like side hustle in a way, if you, I could say, but the cool thing is that it helps.
Give scholarships to our underserved patients. So we funnel that money to these underserved patients and we can give scholarships to them. So it's actually like, it's fantastic. It's easy work. It's fun. And it's, it went way down during the pandemic, obviously. So that income source like almost disappeared.
Um, that was a challenge, but we got through it. So, but I just love that we can actually do the scholarship program with it.
That's so cool. And And in terms of affiliations, you, , have affiliations with the Presbyterian St. Luke's medical center and rose medical center, and then the Rocky mountain hospital for children. What are your affiliations? And do you, , round on patients, if they were to be admitted, at those location,
Oh, good question.
So I did my residency at rose and it's a spinoff of university. so I don't have like hospitalist privileges, but I do go see my patients. What are they called? Social rounds. I do social rounds at hospitals. and then at, I'm on faculty at for university of Colorado, um, teaching staff. That's how I met Alison Edwards, actually.
I think it was through, yeah, she came and did a rotation with me when she was thinking about DBC as a resident. Um, awesome. And then, you know, and then, um, PSL, I'm the, department head of family medicine for Presbyterian St. Luke's. So I get to go to the meetings and kind of listen to the dark side, you know, but no, they're, they're actually really nice and it's nice to be connected to the hospital, just to know what's going on and have updates about the community.
And absolutely the community, focused, presence, as well as the ability to hear what's going on to have your finger on the pulse of the community, especially when you say, like there's more, you know, hospitals than Starbucks, , in your area. So, absolutely. Yeah. And, in terms of going into the future, one of the things that you've been so passionate about is really helping people be confident and understand the DPC movement as a whole, and being an advocate for the movement as a whole as well.
So how do you see DPC growing into the future?
I've already been so impressed with
how quickly it's grown from like nothing to people know what it is. And so the thing that I wanna just implore all of the doctors that are doing DPC and all of you that are thinking about it, once you eventually do it, because just do it, you have to help those on the rungs of the ladder below you.
You have to help them reach out your hand. I had so much support from those few people like Sharon and Ryan. Like when I first started, I had so much support from them and they didn't ask for anything. And I don't think any of us should ask for anything when we're helping our peers, you know, pick a few people to mentor or do some public speaking or do something to help out this movement because this movement will save your life and you owe it , to this movement to save its life and to make it grow.
You're not in this for the money, if you're in this for the money. Okay, fine. But if you're in this, because you love being a doctor and you love having a personal life and you love traveling all over the world, like I do, you have to keep this movement alive and it's your responsibility. So please take somebody under your wing.
Amazing. Thank you so much, Dr. Davidson for joining us today,
that was so much fun. And thank you for being in Denver. It's been a blast.
*Transcript generated by AI, so please forgive errors.






Comments