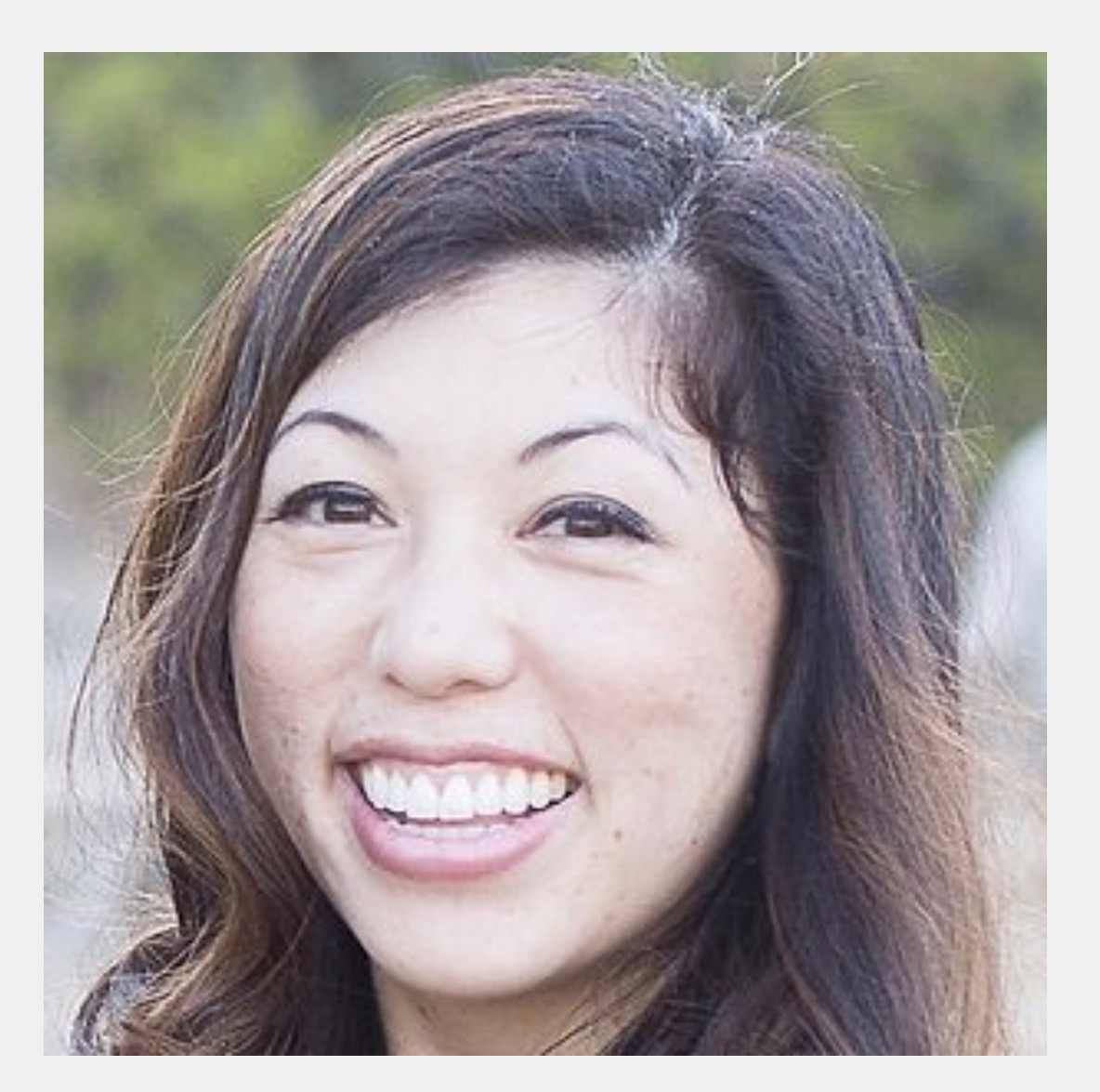
Episode 64: Dr. Nazia Sheriff (She/Her) of Olive Leaf Pediatrics - Orinda, CA
- Maryal Concepcion
- Nov 14, 2021
- 42 min read
DPC Doctor, Pediatrician

Dr. Nazia Sheriff is originally from the windy city of Chicago and moved a few years ago with her husband and two young children to sunny California. She first discovered her love for pediatrics and working with children when she was in highschool! She received her BA in Psychology and her Medical Doctorate from the University of IL at Chicago. During her Pediatrics training at Loyola Children’s Hospital, she was awarded grants for her work in health education for refugee children. Dr. Sheriff then started her career as a Pediatric hospitalist at a Chicagoland based children’s hospital where she took care of newborns and sick children admitted to the hospital. She was the Hospitalist Medical Director as well as the Medical Student Director for many years. Dr. Sheriff created family centered policies that allowed families to be involved in all aspects of their child’s care. Life then brought her to the Bay Area where she has been focusing on preventive and wholistic pediatric care.
Dr. Sheriff believes strongly in lifestyle medicine and has a special interest in breastfeeding medicine, nutrition, fitness, socio-emotional health as well as special needs. She is an IBCLC, is an ACE certified Youth Fitness instructor, serves as medical advisor for Cooking With Kids Foundation, and is a Certified Positive Discipline educator. Her passion is to bring pediatric medicine back to its roots and focus again on treating the whole child.
In her free time, Dr. Sheriff enjoys family hikes, reading, taekwondo, and international travel!
She opened Olive Leaf Pediatrics in the Summer of 2018!


Resources mentioned by Dr. Sheriff:
- For vaccine administration: The Buzzy Bee and the Shotblocker
- Baby scale: Salter Brand scale
CONTACT:
Website: Oliveleafpeds.com
IG: @oliveleafpedsdoc
Call/Text: 9252975573
TRANSCRIPT*
Welcome to the podcast. Dr. Sheriff thank you so much for having me. I wanted to open
with your why, because I loved that when I went to your website, it's such a calming green. You have all of leaf. You talk about the nurturing of a child and your practice as a whole child. And I wanted to get a little bit deeper into the why.
Why did you choose all of leaf as the name of your DPC practice? Well, you know, I really think that, uh, there's so much meaning behind a name. I feel that way about, I felt that way, even when I was naming my own children. And so when, you know, olive leaf was being conceptualized, I, I knew that I had to have a name that had a really personal meaning to me.
And, uh, you know, that reflected the values of the practice. So, you know, I, I knew that we wanted to focus on nutrition, bring in some, like a calming, you know, Peaceful presence. And I just have always been at, I guess, attracted to the symbol of the olive tree. It didn't quite, you know, fit because again, I was dealing with BDS and, and kids.
And so, you know, they haven't quite laid their roots and become a big tree yet. So I, uh, that's where olive leaf was born. You know, it's symbolic of my practice philosophy of like you mentioned, treating the whole child. So treating mind, body, and spirit, the olive leaf has nutritious as well as the medicine properties.
Um, that obviously signified two of the major approaches that, you know, my practice takes healing, the bind and the body. And then in spirit, it grows into a universal symbol for peace and tranquility. So really, you know, my practice strives to help the little olive leaf eventually flourish into a wholesome.
As a parent, you know, that's something that we think about in terms of our kids and who they'll be in the future. And I think that's great that your practice is focusing on nourishing them in all of those departments, so to speak so that when they grow into full trees, when they go into full grown adults, they have, you know, strong roots in healthy nutrition, healthy habits, healthy coping skills, and then feeding off of that.
One of the tabs on your website, it says our philosophy. And I really loved that also because you know, people put it in different words, our mission, our story, our why about us? Why did you choose our philosophy as the heading on your website? Well, I knew that when I was starting all of Lee's paeds, that it was, it was, you know, to attract, you know, families that kind of believed in the mission or the philosophy.
And the philosophy just really encompasses, you know, essentially an entire, like way of thinking. And then therefore also, you know, goes into an entire way of living. And so when I came up with, you know, philosophy, I was kind of thinking about like, you know, Really what, what are the core principles that were important to in my experiences as a mother, in my experience, as a pediatrician and where does that need lie in our greater community?
And so that's where, you know, the philosophy of. Treating the whole child or having a holistic w H holistic approach to, you know, um, just to clarify, uh, came in and also just, you know, in the beginning it was, it was really interesting because I wanted to provide a different type of service for my families.
And I started out with house calls. So I, the philosophy included, you know, house calls as well. And, you know, most importantly, uh, long-lasting change in the world of pediatrics comes only when the parents and the families are invested in your plan of care. So I really wanted to highlight that my care was family centric and not just child centric, because the child is obviously a larger part of that family unit.
So when you say that, it makes me think about. Was mentioned in your bio when you were in Chicago prior to moving to California, you were heavily involved in hospital medicine. And one of the things that you had been very passionate about was creating policies where families were very heavily involved in their, in their kid's care.
And so I'm wondering while you were in that hospital setting, where did you learn about the idea of having a direct pediatric practice and can you tell us a little bit more about that journey to create your own practice? Honestly, it was, uh, it was an accident. I happy one, but definitely an accident.
So I was a pediatric hospitalist for over seven years. Uh, while we were, while I was in Chicago, that's actually, you know, my native city where I grew up and whatnot. And, uh, while I was practicing as a hospitalist there, you know, there were so many. Gaps in care because people just weren't communicating.
Right? The rest of her respiratory therapists were not communicating with the nurses. We're not communicating with the physicians. And so we really implemented a policy and I was, I was the director there. I was in administration. So, you know, I had the ability to go ahead and implement the policies, these family centered policies, you know, rounds and communication and, and whatnot.
And, you know, over time, I, I really was starting to get a little bit disillusioned with the big box medical system through, you know, what I experienced as a hospital as to what I saw with administration. I worked with some amazing human beings, but just the system was so flawed and. Didn't see myself being part of that system in the long run.
And so I was getting that, you know, seven year itch that sometimes be doctors get right at that turning point of our career. And I swear the universe just works in the most amazing ways because right at that time, while I was getting this like, you know, itch, uh, we, we kind of made a sudden life decision because of my husband's career path and an amazing opportunity that came his way to move to the bay area.
This was, you know, literally packed up left family. We had, you know, our kids who were kind of five and seven at the time and really upset with us about the move. And we just were like, Hey, let's just, you know, let's just do this, let's move to the bay area. And I felt like the universe at that time was, you know, Calling to me to just like, you know, or just creating a new path for me.
And when I got here, I was like, okay, I know I don't want to be part of this, you know, the hospital system of a big box medical system. So let me go and try out some solo practices. And I did, and I knew I was like, I want to be in the community. I want to be hands on with my patients. I have so much to offer.
I'd like, you know, like, you know, learn extensively that nutrition and got help and peanut behavior and discipline and all that. I want to do all of that in community pediatrics and the beautiful practices that, you know, I tried out either part time or as locums, which, you know, I had, it was kind of a trial period with the intention of me potentially joining it didn't really have space for that.
Cause they were still traditional insurance-based practices. And so what happened was I was spending. 30 minutes with these like, you know, teenagers that are like Dr. Sharif. You're the only person I've ever told this to, but I cut myself and I do this and it was just because I was just spending time with them.
And I was going way over my limit and calling behind. And the whole system was so frustrating to me. And then I realized that I didn't, you know, make this big life move and this big life decision to, you know, get out of like the comfort of academia of big hospital system, just to, you know, fall into another trap.
And I started doing some research and I came across DPC. I don't even know how I came across it quite honestly. And I was like, this is it. You know, I have to do a non-insurance based practice. And I think I joined like the DPC forums on Facebook or something. And I was like, this is, this is, this is how I'm going to be able to practice Fullscope as, as a holistic pediatrician.
And once he made that decision. Practice holistic care. And to open your, in your own insurance free clinic, did you do any market research? I had done some market research in, you know, essentially the bay area at the time. There were no DPC practices. Uh, actually, sorry, there was one and it was about 45 to 50 minutes away for pediatrics.
I don't think there were any for adults. There were concierge practices, so there was concierge paeds, and then there were concierge few concierge, adults, quite a few of those, but not D not DPC. And I kind of did this like hybrid thing for awhile because I was like, you know, I'm not sure about DPCI that like, is it, is it gonna work?
Like why isn't it here? And so I did this hybrid and I found, you know, faults with that concierge model, even within my own practice. And, and I, I eliminated it pretty quickly within months of opening my practice and I went into straight DPC. So I, I, you know, again, my market needs to just consisted of.
Within, uh, I dunno, like one hour drive, right from the location I'm at it. Just to see what availability there was. And when you initially opened, how did you announce to the community that you were open for? So I did some Facebook posts. I networked like crazy. Uh, I got out there to the birth workers, to other concierge physicians, really just anyone that I could speak to about DPC.
I think I tried some BNI groups. Those I realized were not for me. They are for some people they weren't for me. Uh, and, and yeah, it just kind of organically got out there. I honestly didn't spend a ton of money on marketing. I just, you know, put myself out. And when you opened your practice, did you have a physical clinic or did you do home visit and telemedicine first?
Yeah, so I, um, I knew I wanted to start off lean because this is a big risk that I was taking somewhat risk averse. And so I was like, well, let me just start off, you know, with the, like, I don't know, like $5,000 budget, maybe not, it wasn't even that. And just do house calls and just get all my, you know, equipment and whatnot and, and start off that way.
So I did house calls for about a year and I was growing and I was getting. Really tired of driving. Quite honestly, I loved seeing babies, especially for the first time or, you know, essentially for like the first month in their home, because I felt like it's important to provide a new family that service, but past that, you know, I didn't really feel like it was necessary.
So about a year after I opened, I actually opened up my clinic. Uh, and it's, you know, five minutes away from my home. I chose a path of convenience, quite honestly when opening up my clinic, but yeah, five minutes away from my home, five minutes away from my kids' schools. And it's just, you know, like just, I love it.
Like it's, it's my, you know, it's my little sanctuary away from home sometimes. Awesome. And when you mentioned that fatigue from driving at happened, did you have any strategies or thoughts when you were opening and you knew that you were going to open lean and do home visits as to how you would accept patients?
Like, did you have any I'm only gonna do. The patient's first from this radius and then work out words from there, or how did you do it? Absolutely. Yeah, because I, I believe, you know, part of practicing, uh, preaching holistic care is that you also have to practice it in your own life. Right? So I have a family and they're obviously a very important part of who I am and my identity as, you know, being a mother.
And so I knew that I couldn't stretch myself too thin and they still had to be available for my own children. So I limited it initially to about 20 minutes. Um, the bay area is a little bit naughty because like, you know, you could be driving like three miles and it might take you like an hour. So, you know, I've limited initially it's about 20 minute driving radius.
And then sometimes I'll still extend that to like 30 minutes, um, especially for newborns, but, but that's kind of my max, I don't ever go past 30 minutes. And I even from the beginning, you know, I really wasn't planning on going any further. And on your website, you list the areas that you service within that 20 minutes, but it also says, and more so it specifically reads, uh, Berkeley, Oakland, Piedmont, Lafayette, Orinda, Moraga, Walnut Creek, Alamo, pleasant held Danville and more.
And so I'm wondering if you make exceptions, what usually falls in that bag of, and. Yeah, that's uh, and that I actually initially didn't have that and more, and then I realized that I was getting calls from these, like, you know, really sweet, like somewhat, you know, really excited families about my practice.
And so, you know, oftentimes, um, right after baby is born, I'll, I'll sometimes extend, you know, my services outside of the cities listed and see the babies at home for like about a month and then have them come to my clinics. So the, you know, again, it's per my discretion, but usually if there's very sweet sounding families that are super interested in my practice and believe in the philosophy, I, you know, I do tend to be, you know, a little, a little lax about that and you can, it's your practice.
Absolutely. That's awesome. I, I think back on. My, my former attending, who's a pediatric hospitalist. He had a baby on his service that lived 45 minutes away from me and the baby needed a circumcision. And so came to my clinic and I was like, oh my gosh, you drove all the way 45 minutes from where you live to come see me.
And they were like, yes, because your, your PO your friend in the hospital, uh, recommended that we come see you. And that, that family, I just think about them. When you mentioned, you know, there's this special families who are so excited about, you know, being in partnership with a physician who actually cares for them and who takes the time out to really give them, you know, the, the time that they need to address concerns, especially with newborns. Absolutely. It's I think one of the beautiful things about having a practice like this and, and yeah, and it, you know, I think families that feel akin to the practice also, obviously self-select and use somehow self-select them.
And, you know, the universe just kind of makes everything work out and thinking back to those earlier days, whether it be the early days. When you started what were some of the growing pains that you remember either good or bad? Yeah, absolutely.
So, I mean, I think the biggest growing pain was that because I was getting a little bit conservative about marketing in the beginning and I'm not originally from the bay area, just getting patients, you know, and setting up, you know, I had all the system processes set up, uh, in place and because I'm, you know, have focused a little bit on detail in case you couldn't tell from my website and not, you know, like pounding that pavement and not seeing that return by the way.
I think that was, that was pretty painful, but, you know, Consulted with other paeds DPC doctors across the nation. There's like a small network of us. Um, that's growing actually, which is amazing. And everyone had the same story, even, I think family practice and adult DPC docs kind of all said the same thing.
So yeah, that was, that was a little, a little tough in the beginning. And I think, you know, my practice still cycles through that, right? The pandemic we had to switch up things, you know, convert to tele-health impossible, but still keep, you know, some in-person visits. And so that it was a different type of growing pain, I think.
Um, but the, the, again, you know, going back to it, I think what centers me, and you've mentioned this before, is that really like, this is, this is my practice. If something isn't working, if something is, you know, so painful, I can always amend it. So, so I am constantly changing my goals or, you know, certain ways I do things and whatnot, just to.
That's awesome. And as your patients have joined your practice, what's the most common way that they've actually find you? It's actually been referrals through, uh, you know, my, you might not work. A lot of birth workers have refer me. They're really like, kind of like my, you know, a little bit more gentle way of care, especially with babies.
And then I actually, uh, Google search. So I, I actually have a question on my form, my intake form, as well as on my contact form, just asking like, Hey, how'd you hear about us? Uh, just to find out specifically that, so it's either birth workers or Google search Yelp. And do you have any specific tips on how you manage your Google business profile and your Yelp profiles?
Yeah, I, I don't have any amazing tips other than, uh, well, actually I have one centering tip. As soon as you start getting patients, ask them to write you reviews. I was very bashful in the beginning and I think I went like a whole year plus or something before I asked any of my patients for it. And they would all say like, oh my goodness, we love your service, blah, blah, blah.
It's also great. It's so different. But I just, you know, as doctors where we're not used to accepting that praise and we're not used to like showing, you know, uh, that praise to the outside world when we do get it to sharing that praise, I guess I should say. So I think just trying to get reviews right from the beginning, being bold and confident in your service.
And the, the value that you provide that that's going to help attract other patients, it's going to help your SEO rankings as well. Other than that, just, you know, posting on Google, uh, whenever you can. I think that also helps things and, and yeah, that's, that's pretty much it, other than that, like my profiles on both aren't anything special, they're just basic stories about me, but you know, I, I've tried to recently work a little bit harder on getting reviews.
And can you give us an example of the dialogue you have with patients when you ask for. Yeah. So this actually took me a really long time to, you know, must have the courage to ask my patients, but typically, uh, you know, as you know, and I don't ask all my patients, I'll, I'll just, you know, when I remember I will, but typically I'll just say, Hey, you know, you know, they'll, they'll be leaving, they'll say something nice.
Like, oh my goodness, thank you so much. This was such a great visit and blah, blah, blah, feel so calm or whatever. And if I see that window of opportunity, okay. Take it now and say, Hey, I'm so glad you feel that way. I love having families like you in my practice. And you know, I don't hire any like big marketing firms or anything like that.
So I would love it if you would share exactly that in either a Google or Yelp review, and I'm happy to send you a link if you'd like to make it easier. And they're always, you know, usually if they're like, oh, sure. Of course, no problem. That's great advice. And I feel that because I'm sure everybody has seen a Google or Yelp review.
When you read those positive reviews, it's like all five stars because you know, people, when people love practices, especially DPC practices, they go berserk like in a good way. I mean, they're, they're literally the walking and talking billboards of your practice.
And so I, I, I am really glad that you shared that. I hope that that helps others, especially those who might also be in that boat of dot really sure about how to ask or I don't really like asking people for reviews, it goes back to the idea that DPC is building relationship based medicine.
And if you are in a relationship with somebody and giving them the best care, you definitely deserve kudos where kudos is. Yeah, no, absolutely. I think that, you know, just really honing in on those relationships that you've worked so hard to foster and like you mentioned, letting them do the advertising for you.
I feel like it also just draws, you know, families a little bit more organically than a marketing company or a big box from sure. And I'm sure a lot of the legwork is already done in terms of understanding what your practice brings to your patients, because the potential families or the new families are hearing organically.
Like this is what my kid, you know, had it, his or her visit with Dr. Sheree. Yeah. Oh, it's so great. Because whenever I get, you know, patient inquiry calls, uh, from a patient, from a family that was referred by one of my patients, it's the easiest call ever, because, you know, I'm like, oh, so, you know, have you had a chance look at my website and you want me to go over my philosophy?
And they're like, no, no, no, we got it. You know, we are friends with so-and-so and they told me how, uh, you know, how amazing things are, like, how do I sign up? And it's, it's that easy. So it's, it's just, yeah, it's so seamless. And have you come to a point where you're putting people on a wait list? I think I'm getting pretty close.
And again, you know, I think my goals have shifted a little bit just with, with the pandemic and just really, you know, being able to, to balance things in, in my life overall. So I've condensed my goals and I'm getting very close to putting people on a wait list, especially after like that last couple of months.
That's, that's definitely in the works. And now with that said, how do you structure your week in terms of the amount of home visits and the number of clinic visits? Yeah. Great question. So I limit home visits now only two newborn to three month olds. So that cuts down immensely. I also make special exceptions for kids that may have be, have some special needs or a lot of anxiety.
You know, they, I think also deserve that, you know, the doctor coming to them. So I would say probably 30 to maybe 40% of my week is house calls and the rest is, uh, clinic. And I, you know, I try to carve out at least one day a week, whether it's a Monday or Friday as my admin day, sometimes both if I'm lucky and do heavy lifting week, and again, that's the beauty of DPC.
You know, I'm able to kind of flex in and out. And, you know, when my kids have like busy, like Tuesday and I have to be that room mom or whatever, then I'm able to, you know, schedule around that and. That's just great. I just love that. I mean, I, I think back on, uh, one of my friend's kids had a school performance, you know, like a kindergarten school performance at two o'clock in the afternoon, and I'm like, who can go to that?
DPC doctor could go to that for sure. A hundred percent, a hundred percent yet this week I'm on carpool duty. So I am picking up everybody at 2:00 PM. My clinic is closed for business at 1 45. That's awesome. And do you ever have cases where you do have a surge of need in terms of like cold and flu season or the pandemic where you have to do extra hours of care than you're normally used to?
And how do you balance that with your family life? So, you know, one of the things about being an entrepreneur is sometimes these surges happen, right? And it's not, you know, like a very clean, linear, exponential growth. It's like, Ooh, you know, I know you guys can't see me like on this podcast, but I'm basically doing a little wave with my hand.
Um, but yeah, it goes up like that. And so I've learned to like embrace the surges to the best of my ability, pull in some extra hours after the kids go to bed with, you know, charting or logistics or whatever needs to get done that week. I really utilize my admin. I have a fantastic administrative assistants and we've streamlined some processes.
So, you know, she does a lot of heavy lifting with me that week. And I try to, you know, put as many responsibilities on her as I can. And then I know that the surge is not going to last forever. So I mentally prepare myself just to kind of get through like that week or month or whatever that looks like.
And then, you know, things will kind of always balance out after the. And can you share more about this assistant that you have? Is this a virtual assistant or is this somebody who is physically in your office? Yeah, so she's California based, but she is virtual and I, you know, I've toyed with the idea of hiring somebody to be in my office, but I really haven't had that need quite honestly.
And she, she does everything, you know, nonclinical. So all of my, you know, I don't know, like onboarding patients, you know, chart like reviews or, you know, like filing things, faxes, you know, some phone calls, all that stuff. So she takes care of all of those things for me. And, uh, and even, you know, like training her was a bit of a process she's been with me for it'll be a year actually, uh, at the end of the summer.
And you know, the first few months it was, it was a little bit tough, but now she's amazing. And I don't know how I could function without her. Absolutely. And in terms of getting. To a place where you and your assistant are able to work seamlessly. What are some of the key things that you found helpful and necessary in that process to get to where you are?
Yeah. So here's the game changer. I actually had her make her own SOP manual and, and we, I mean, we worked on it together, but she was, uh, pretty much responsible for it. And after that, you know, I edited all her responsibilities were just all laid out, listed out my expectations, you know, of, of how I wanted things done.
And really after that things took a turn for the better. So I highly recommend that everybody do that. And again, for me at that moment in time, I didn't have time to make it for her. So it was one of her responsibilities to make it for herself, with me overlooking. That's genius. And just in terms of, especially if there are early entrepreneurs, SOP is standard operating procedure, but yes, I think that it's also so important.
I'm sure for you, because as an entrepreneur, it helps you with your time and not flailing all over the place because you're, you're working in that SOP that she set up that you've embraced. Yeah, absolutely. And even that, you know, even our SOP is right. Changed all the time. It's, it's not, uh, it's a fluid process.
So, so it's great to have the ability to modify that, um, as my practice changes. So for example, you know, my onboarding process has, you know, had to be tweaked. It was, it was filled with inefficiencies. And so we revised that just to, you know, come up with a better system of how. We could like get through patients, you know, uh, get them all set up and, you know, uh, I'll tuned out together.
So, so yeah, it's really great to have stuff in writing and I'm big into like lists and, you know, checking things off. And so is she, so it works really well. You don't necessarily have to geek out over this, but if you are geeking out over this and questioning, if you could do DPC, I'm going to say absolutely.
Yes. Because, uh, this, this idea of constantly being able to change based on your needs. I mean, yes, we do it in everyday life, but I feel that when it's extended to the, the practice of medicine, I just find that so exciting because just like you're, you're talking about, you can, you can have hours that you set, you literally can change your SOP.
Like this. The next sentence I type is my new SOP and I'm making it because I'm typing it. Not because I had administrators telling me that this is how it's going to be done. Yeah, absolutely. And that actually applies to all aspects of, of your practice when you're, you know, when you're in the setting, because whenever I start to feel that my practice is becoming stagnant or, you know, there's lack of growth, I find that it's it's because I have to tweak something and maybe like a little tweak will either make me enjoy the practice a little bit more, or, you know, start having it grow in, in a more like natural direction.
So that's the other beauty of DPC, you know, that being said, like, I'm always, you know, people call me for advice and whatnot about specifically for pediatric TPCs like, you know, I, I do also want it to. Paint a very realistic picture, uh, because I am also like a realist at the end of the day. Like, it is a lot of hard work that, you know, most of it is very enjoyable, some of it not, but, but yeah, it is a lot of hard work and for some, um, growth might be slow.
I, you know, especially my first year, I definitely had slow growth and with clinic again, that was another game changer. As soon as I set up a clinic, I started getting patients driving from like an hour away, you know, to, to come to my services and I was able to know, expand my patient base because of that.
Now, in terms of your assistant, I want to take a step back even to how you found your assistant. How did you end up getting in touch with somebody who could be an assistant in a medical.
Yeah. So, so I actually went through a couple other virtual assistants through a company and they, they just did not work out. We were not on the same page. And then I have a buddy who is a lactation consultant. I work very closely with her and she said her admin was looking for more hours. So it just, you know, when I interviewed her, it seemed like a great fit.
She was already like, you know, HIPAA compliant. She was already familiar with, you know, moms and babies. She'd never done pediatrics, but, but she did have like a little bit of background and medicine and yeah, we, you know, we talked and it was a really informal interview because for me, it's also about just like, you know, I can probably tell within like the first 10 minutes of a phone conversation, whether it's going to be ready to fit and yeah.
That's great. And you know, it just, it goes back to when you were marketing and you were just telling everyone you could about your practice and how it organically grew from there. I love that. That's how you've ended up finding your assistant. And it makes me think about Dr. Natalie Gentilly, who had been working with a medical student and, you know, basically exposing her to DPC.
But similarly, if you had somebody who wasn't even necessarily an assistant, but was a really good organizer or somebody who was willing to learn the art of being as being an assistant, I mean, as you talk with people, you literally could find somebody that you could train and groom from the get go.
I think that you don't necessarily have to have that coding background to be any coding background, um, to be an assistant that's effective in doing administrative tasks. Oh, yeah, absolutely. And, you know, I was fortunate where she did have a little bit of a medical background, but she, you know, she didn't really know anything about pediatrics.
And so that was a little bit of a training process, but yeah, really anyone who has great organizational skills, who has, you know, who is just like a quick thinker and a quick learner, they could easily do a virtual admin assistant job. Absolutely. Great. I wanted to go into more detail on your onboarding because, um, you talked about that your assistant is doing the heavy lifting when it comes to onboarding, but what does it look like from the patients.
Yeah. So the patient experience is very important and the patient experience is only through me. So my admin does all the stuff in the background, but for me starting my pediatric DPC practice, I really wanted all the clinical stuff and the patient experience to be directly with the doctor, because that's what people are signing up for.
So all the, you know, initial welcome emails come through me. I do customize them. I have a general template and customize them to each patient depending on what their scenario is. If they're about to have a baby, if they already have a baby, you know, they have a ten-year-old and yeah, I mean, it's, it's really, really pretty easy.
We do have everything is online. Big proponent of paperless for those practices that are considered, haven't gone paperless, please do it, will make your life so much easier. And it's so much friendlier for the environment. And, uh, so they just fill out an online registration form. All of my policies and procedures are on there, but I also just talk them through it as well prior to signing up, just to make sure that they clearly understand everything.
And, um, once they say no, they get a welcome email. We, you know, uh, ask them to have any questions. And then we just schedule our first visit. The backend of things is like, you know, a little bit more logistically based in terms of getting records or billing records, you know, blah, blah, blah, all that stuff, scheduling.
And that's all, uh, what my admin does, but as soon as they sign up, as soon as they fill out the form and I tell them that they're welcome to text me any questions. So sometimes I'll have, um, you know, expecting moms say, Hey, can we like schedule a quick chat before I go into labor? And so, and I love that because then I can start.
You know, enter it. Like I can, I can start like guiding them right from the beginning before baby's even born. So, so that's been, that's been fantastic work that in terms of contractually, when a baby is yet to come out, do you sign the parents on as patients? Or how does that work? Yeah, so no. So the, so the baby is signed on, you know, as, as expectant, as like in utero, they initially have like an enrollment fee that they pay for me.
And then from that, there's like a contract that's made between myself and the guardians right. Of the baby. I don't give any like specific, like, you know, I mean, I do give some advice, but I don't call it medical advice. I call it more of like, you know, like coaching and with the caveat that all the advice I'm giving them is for the health of the baby who is ultimately going to be my patient.
So it's never surrounding mom's health. It's always associated with. You know, upcoming baby and, you know, from, uh, my, my, my standpoint, my malpractice standpoint, that that's like totally fine. I think that's great because it doesn't limit the care to only moms who are scrambling to find somebody after they're discharged from the hospital.
Absolutely. Yeah, absolutely. I, you know, I think the bulk of my patients actually do sign on during their prenatal period. And I encourage that. Uh, just because, like I said, we can, you know, start talking about breastfeeding right away and we can, you know, sometimes being in the bay area, they have questions about vitamin K or Hep B vaccine or what the hospital experience is gonna look like during COVID.
And, and so I'm happy to guide them a little bit. Right. But from the start, and now I want to touch on your IB CLC training, because your current, as, as of this recording, you're still working towards getting your certifications. So I just took my exam last Tuesday and I'd spend, I don't know, like a decade since I've taken a standardized exam.
So that was quite fun. And yeah, I, it's just a matter of, you know, um, getting results and hopefully, hopefully I passed and, uh, then I'll be credentialed as an IBCLC. You know, that being said, it really is just something on paper because my experiences up until this point have not changed from before to after Tuesday, I've been practicing breastfeeding medicine for, well over a year.
Now I have that friend. Who's a good friend, who's an IP CLC. And I actually did a bunch of shadowing with her just to get more comfortable and hone in a little bit more on my breastfeeding counseling abilities. And so I've been doing that, you know, that plus all the reading and training that I did for the IBW CLC tests really, I think has prepared me to prep.
And that's, that's one of the questions I wanted to ask in terms of, you mentioned shadowing because they know that there's a certain amount of hours that you have to get, uh, to go along with the test for certification and are credentialing. And how did you build those hours in addition to shadowing into your practice?
Yeah, so, so there's, there's like a window of like, I think it's like three to five years or so. I, uh, grandfathered in some hours that I had as a hospitalist because we did newborn nursery and, you know, a ton of breastfeeding counseling, although it was really rushed, but still we did it. And, uh, and then just working as a general pediatrician.
So there's a few different pathways you can take, you can either do the mentorship pathway. So if I were to do that specifically with this ID CLC, I think that would be like maybe like a hundred hours or something with her, or you can do, you know, as, as physicians, we can actually just do pathway one versus a primary pathway, which is the one I ultimately ended up doing that being said, you know, I really, I want to be the best, right.
I want to be a pediatrician who has that, you know, knowledge, but I also want it to get the next peer experience from an, a true IBCLCs standpoint. And so I felt like that shadowing and the mentorship I received from my. Super duper helpful. And what are some best resources for people to know about?
Because they know that like I Abel's out there and I have fantastic. Oh my goodness. It's fantastic. So if you want to get your hours, you can use, uh, e-health learning and that gives you like your book hours. Uh, I think you can get like up to a hundred or something like that. And, uh, there's also something called LER lactation education resource.
I think that's what it stands for. But most people use e-health learning and I able, I attended their conference last September and you know, that, you know, after like shadowing the lactation consultant and actually I have a couple other friends, you know, Friends too, who are lactation consultants, who I sometimes refer to, or, you know, just kind of chat after like kind of hanging out with them, shadowing them, and then going to the able conference.
I was finally like this, this is breastfeeding medicine. These are my people. This is, you know, this is how I want to practice. So I highly recommend the conference to anyone. Uh who's. That's great. And I don't know how they will shift into the future, but so far they've done little mini conferences like every, every other month or so.
And the topics are definitely, they're not static. They're, they're constantly changing and they're constantly updating the medicine behind the, the, the presentations. And I love that. They're they make it clear, like this is physician focused learning, and this is patient focused learning, but we'll, I'll make sure to include the able link on your company blog, post on the website.
So I'm glad you mentioned that. And I just, I really love though, that you are, , as you mentioned that you're talking about breastfeeding, even before the baby has come out because it's for the baby's health. And I just think that, when I look, when I think back on my experience as a first time, mom, how many patients that I counsel.
On the wards, on the postpartum war, it's about breastfeeding. How many, you know, articles that I read, how many presentations had I been to? But when I actually had a kid, I distinctly remember our attending who had trained us and who had also delivered both of my sons now. Um, she walked in and I was feeding my son
and she was like, what, what are you doing? And so, you know, I, I really, I really think. That's wonderful that you're bringing breastfeeding medicine, not only as a mother, but also as somebody who clearly supports not only breastfeeding moms, but also kids who are taking formula or both. And I wanted to highlight that because you have this amazing picture that I'm going to put on your blog as well, where, uh, for the listeners, if you haven't, if you haven't visited her, uh, blog yet it's two slides that can join at the bottom.
And one slide is labeled formula at the other slide is labeled breast milk and there's two kids sliding down the slide and what the confluence, it says that they both end up at the, at the point of eating crusty French fries off the floor of the minivan. And so I love that, but it's, uh, you're, you're, you're going back with that picture, in my opinion, to.
To that idea of your philosophy that you're treating the whole child, whether they had one or the other. But I also think that just your experience and the fact that you're focusing on breastfeeding medicine is also great for those moms who are able to breastfeed or who have questions about breastfeeding, because that's where I feel that even as good as the lactation consultants are in the hospital, their time is so is so truncated.
As I feel fee for service visits are in primary care because you're exhausted. You don't know the last time you slept, you don't know you're your own name sometimes in the hospital. If you choose to deliver in the hospital and then someone tells you, this is how you breastfeed in 20 minutes. And what, what tools do you have after?
I mean, literally that's, that was my experience when. My attending walk-in and questioned, like, what was I doing with my son? So, you know, my, the, the breastfeeding medicine aspect of my practice, you know, comes with like, just like a deep sense of like empathy, uh, for, for my patients.
And that's really why I wanted to expand on it. Really, my entire practice is in a way, like my own wishlist of everything that I wanted, you know, from, from my pediatricians while my kids were young and they, my pediatricians were wonderful human beings, but, you know, again, what that 10, 12 minute appointment not really being familiar with breastfeeding, I really felt like I needed more support.
And I realized, you know, I had to do so much learning and, and, you know, research and all that stuff on my own, or seek out resources on my own. I thought like how is a lay person? I'm a pediatrician and I can't get this straight. How is a lay person able to handle this all on their own? So the goal for my practice is really to be part of that village specifically for like new moms and young families, and really support them through this tough time.
And my breastfeeding journey with both of my children was not easy and I didn't, I kind of scrambled and I, you know, had to figure it out and I didn't have the greatest support. I really didn't even know there was that much support available and it was, it was a bit messy. And so I know I want to prevent that for other women, if they so choose to breastfeed, I want to try to like, you know, ease their frustration and just be, be there for them.
I want to go into more detail on the fact that you're a certified positive discipline educator. And the other part of your bio that I absolutely loved was that you are conscious about socio-emotional health. And so I wondered if you could share about how your practice encompasses. Those two aspects of your training?
Absolutely. So, you know, I loved, uh, in my younger years to like geek out on psychology. In fact, that was my undergrad major and I just had a profound interest even starting from high school. I like, you know, like all AP psychology to up. And I wasn't sure if I was going to go into pediatrics or child psychology and because they were both so fascinating to me and the on medicine one, just because, you know, I, I'm also a science nerd as well.
So, so I incorporate, you know, a lot of, of maybe my, you know, I don't have post bachelor's psychology training, but whatever knowledge I do have, I do incorporate that into my practice. I I'm very clear with patients, you know, and telling them I'm not a therapist nor do I replace the therapist, but I can absolutely, you know, coach you during this time, you know, again, being.
Struggles as a parent myself, I was like, how can I solve this? And so I just started reading a ton of parenting books and I came across an opportunity to get certified with like positive discipline. It's uh, you know, again, it's, it's a type of, you know, parenting approach that is based on, uh, Jane Nelson's work.
And I, I realized that not only could that benefit me as a parent, but you know, later on with my pediatric patients as well, if I were to practice community pediatrics. And so that's, that's really how that came about. I so much of what I do comes from just, again, my experiences, not only as a parent, but like just my special interests, uh, of my past and discipline and psychology and whatnot, and just, you know, hearing my, my patients stories and adjusting plans.
As needed what works for one, obviously isn't going to work for the other, but just kind of there's over time, you start seeing patterns emerge, right. Especially during different developmental stages. And with certain family dynamics, you start seeing these patterns emerge and you're able to counsel your, your families a little bit more effectively based on that.
And I'm sure just going beyond the time that you have the fact that you have relationships with these families, and you've seen that family dynamic develop over time and how, you know, that changes you've seen, and you've been able to see those changes for each family as the kids grow older. Absolutely.
Yeah, absolutely. You know that plus like they, my, my patients have access to me. Right. So it's not limited just to our appointment, which is typically an hour long, sometimes a little bit more. Uh, but it's not just limited to that. Like, my patients are able to email me, text me, call me, put some, anything urgent and, you know, Again, all of that, that, those access points foster the relationship as well.
And me getting to know the families equally. Well, you have your teen patients texting you if they need some, they need medical advice. Yeah. So I don't have a ton of teen patients and the few I do, I, I have not get, you know, written a waiver or anything like that for parents. So they are not allowed to text me, but the parents always are, but I do, you know, tell them that they can like schedule an appointment at any time.
And we don't have to have, you know, the parents in the room if they don't want. So, so, yeah. And, and in your practice, to what extent do you discuss contraceptive? You know, quite honestly, my older patients where I would even discuss that with our mail. And so I, I don't prescribe OCP to them, but obviously we have a discussion on, you know, safe practices and whatnot, and then the other ones are not quite there yet.
Gotcha. And what about vaccinations? How does your practice handle vaccinations, especially pre childhood preventative vaccines? Yeah, so we, we try to follow the CDC schedule. That's the one I recommend being a pediatrician. You know, that's always a best practices, you know, obviously are always number one.
You know, that being said, I do have quite a few patients that prefer to be on a slower schedule or an alternate schedule. And one of the mantras of my practice is to provide that like, I guess, gentler, personalized care, because I think that. Approach quite honestly works best for some of my vaccine, hesitant families.
They really appreciate that. I hear them out and then I'm not dismissive in the end. Some of them actually just ended up doing the CDC schedule or they, you know, you know, vaccinate a little bit more quickly than they would have thought otherwise, just because they, they do feel like they can trust my expertise and my judgment.
Again, going back into your teen care, because I think about how in fee for service, sometimes frustratingly, my teen visits are the fastest visits because I have a person across from me who I haven't seen in two, three years who comes in because they need a sports physical and they just do not wish to partake in conversation.
And so I wonder, you know, because I know your kids are not teenage teens yet. Correct? Uh, mine are not my own kids. I have a tween. I have, yes. with you having this relationship with the teens? And I know you said you don't have a lot, but how do you handle their care when they're not necessarily seeing you that often, do you reach out to them?
To, uh, make sure that they know that they have an open platform. I know you said the parents are the ones who contact you legally, but how do you deal with your teen population with regards to that relationship that you have that open relationship that you have? Yeah. So I think, you know, part of it goes again, back to, even though they're only seeing me maybe once or twice a year for the super healthy ones.
Right. I think the fact that we spend like an hour plus at these appointments and they're with me the whole time, there's not a, you know, an ma taking their vitals or like the nurse giving them their shots. It's it's me like doing everything. You know, as I'm doing their vitals, we're chatting and we're having Danter and whatnot.
And they know that parents have to step up for a little bit and, and I just try to get it become very, very approachable. Uh, and you know, again, I have to tailor my, uh, my communication style, you know, between like sometimes between genders, if they have a gender preference or, you know, obviously between ages and whatnot.
Um, but yeah, just the fact that I, I think I really listened to them, uh, during these appointments, especially, you know, uh, even when parents are there. I make it a point to really make eye contact with the patient. And I don't have them sitting up on my treatment bed or, you know, or whatnot. Everyone's just actually sitting on a couch.
So my clinic is also set up in such a way where it's, you know, it's kind of like a living room and then there's like a treatment bed and some like medical supplies thrown in on the side. So I think that environment also just like facilitates comfort. I was very deliberate and the colors and, you know, the environment that I chose as well.
And, uh, and, and they know that they can get in touch with me if, if they need me to. The other thing that I do is if there's things that need follow-up, I don't wait the full six months or a year. I'll just schedule like some of my team patients. I see them every three months, because maybe there's something that we're working through and, you know, each appointment doesn't have to be a gazillion hours long, but they know that there's a follow-up scheduled.
And, and I, you know, I like having that frequent contact, if there's something that, that needs to get accomplished. Great. And in terms of doing things like keeping in touch with your patients, what are the communication tools that you use in your practice to do HIPAA compliant, texting, or to do even the electronic medical record?
Keeping? I have a patient portal through my, my EMR that I use. And I also give, um, because you know, my practice is meant to work for families. So some of my patients prefer to use that, but then other patients actually prefer. Texting and emailing. And I'm very, very clear in all my contracts and policies, procedure forms.
I have them signed in the beginning and I had mentioned it, you know, our first visit as well. But if they choose to communicate me via text or email, it is not HIPAA compliant. I mean, it's, it is sorta HIPAA compliant, but it's not a hundred percent the best way to approach that is through my patient portal.
So they signed a waiver that if they do, you know, initiate a text or an email that they're acknowledging. You know, we've in big box medicine. We have to have like all these like set barriers, right. Because we're so concerned about potentially, you know, we're practicing defensive medicine more often than not even if it's subconsciously the beautiful thing about having a small practice, a boutique or DPC practice is that, you know, there's that innate trust that happens between families and doctors.
And so I, you know, I don't let the litigenous aspect of medicine really guide my care. Again, it's always a pain point for me whenever I have to log on to like my hundred portals, just to get access to like the nurse to maybe we'll talk to the doctor and I wanted to eliminate that, but I also wanted my patients to acknowledge that that's not completely HIPAA-compliant.
And so if they're okay with it, then they need to, you know, sign the waiver and most happily do it. They, they actually are, you know, completely fine with that. And thank you for sharing that. And I wanted to ask more about. The tools of your practice, because you do do home visits. Can you give the listeners a little peak into your best tools that you carry for your home visit?
Oh my goodness. Yeah. So this, this was such a work in progress and I've gone through so many doctor bags, you know, from like roller or tough bulls to like, I don't even know, like toads and whatnot, but I have a great system now. And I think after COVID I finally like perfected it, but yeah, so I, I have a backpack because it allows me to be hands free that I carried the bulk of my tools in.
And, uh, and so that has, you know, my essential, so it has my stethoscope, my oldest scope is the scope has, uh, you know, my. Like a measuring tape, ripe or head circumference or any, anything else I might need to measure. It's got a thermometer and, you know, a pulse-ox right. So I see babies. And so it's important to have a pulse-ox ready.
And I think that's kind of the basics of it. My, I have a bunch of other stuff in there that, you know, I can't recall off the top of my head and then I have a baby scale, as well as it BB measure mat that I actually then just carry. And then I have a vaccine cooler, which I actually, you know, it, it was, I got off of eBay and it was like designed for like, you know, who transport of vaccines and like, you know, rural places and keeps vaccines good for like 12 hours or so.
So, so those are all my tools, but the hands-free is key. I used to have a duffle and it, you know, didn't work as well as I thought, but yeah, that's, that's essentially it. I think those are probably the most important ones. Fantastic. And I wanted to ask you some of your best recommendations for specific tools that you use in your practice, because everybody has their favorites, but I wanted to ask you yours.
What is your best tool for your clean. Oh, quite honestly, uh, D Broxson a curate. Uh, I'm, I'm, that's simple gal. So I, I don't go beyond that. And, and you know, the other nice thing about having this practice is that if, if the child, so I try not to make the experience miserable for the child, because I know that I can always see them in a day or two, and parents don't want to make my visit a miserable experience for their child.
So if it's, if they're, you're so impacted and it's not anything urgent, right. That I need to look at right away, I have the luxury of just de bruxing a little bit or telling, you know, parents to detox on their own, or, you know, just maybe throw some water while they're in the shower or the bathtub or whatever.
Right. I'm at home and bring them back in a couple of days. And we'll take a look at that year. Again, that's if like the curate and all that don't work. What about best tool for foreign body of the. Oh, so in a flailing child, tweezers, even if they're plastic won't work, mother's kiss is usually great. So that's, I think that they don't even need to see me quite honestly.
I've had patients just do that, like on tele-health, like, they're like, oh, they stuck something up the nose and you kind of, you know, walk them through it. But yeah, I think that's probably it. I don't, yeah, I haven't really other than plastic tweezers, which again are not my favorite that that's probably it.
Best tool as a pain distractor. Uh, so if we're talking specifically vaccines, I have a couple of different options and I kind of let families try it out. I have the little buzzy, which is like, basically a little like ladybug or bumblebee, depending on what you get that you put on the skin and, you know, kind of like, you know, buzzes and stimulates, like, you know, the nerve endings that are proximal to the area of the vaccine and supposedly they feel less pain.
Um, what I've noticed is in babies and tellers, like they hate it. They're they're, you know, they're like, what is this like vibrating thing that you're putting on my skin? So it's fine for older kids, but that's just the simple yellow shot blocker is great for vaccines. Other ways. Uh, I have this like little, this little handheld bubble maker.
That I think I got from like target and I have one in my car for home visits and I have one in my clinic and I usually have one parent, like, you know, do use the bubble maker while you know, the little toddler watched the bubbles as I had missed her vaccines. And then if it's someone who's has a lot of anxiety, quite honestly, I, uh, I tell parents that this is like the one time where I am completely okay with screens, you know, like child life, we'll use screens for lab draws and things like that.
And, and it's, it's okay. Like bust out that iPhone and put on your, like your favorite, you know, I don't know, Daniel tiger episode or something. Yeah. I, I definitely employed screens when I had to do sutures and a kid that was a, that was. Very tough until I, I don't, I think it was Dora the Explorer that we had on our screen, but yeah, I hear you when, when it's, when anything to get the job done is, is what the job calls for screens can definitely help.
What about best band-aid? Oh, I quite honestly, I don't even know what the brand of the bandaid is. Cause I alternate between band-aid and MCAT, whatever McKesson has, but, but you know what, I, obviously, I, you know, get like, like latex free and all such band-aids, but for me what's more important is the visual aspect of it.
So right now I have these like cute little tidy band-aids that all my patients are super excited about. And I have no idea what brand it is. I think I got it off, like, and our McKesson or Amazon or something. And if you haven't mentioned it already, what is the tool that you could not live without in your practice?
From my line of work, probably my baby scale. Like I, that thing gets lugged everywhere.
I actually have loaners for families to some that I give out. I would say my baby scale, but if, I guess I'm talking about level of importance by studying. That's awesome. And what brand of baby scale do you use or do you use just a folding one or what, what type of, so I actually, the one I do for house calls is a very inexpensive one because I have like three or four of them that I loan out to families, especially in the beginning.
And it's just like a Salter brand that you can get off of Amazon. I've, cross-checked it with my more expensive clinic one and it's pretty, pretty accurate. And so, so yeah, I sometimes families, if they ask me for recommendation, I just tell them to get that before baby's born. Wonderful. And something that I, I loved learning about you was that
you had been a host of a clubhouse room recently and you were, and I wanted to ask you, would you recommend physicians harness the power of clubhouse and what were you, what was your experience using it in general? Yeah. So I, uh, I actually really enjoyed using clubhouse and I think if I had more time, I would be on it a bit more, but, you know, with, with the whole world being on zoom and us just having complete zoom fatigue, I thought that clubhouse was just really refreshing and filled a need for people, you know, similar to this podcast, just to have these, like, you know, these conversations, right.
And these like informal chats, it wasn't visual at all. So definitely more for, you know, the auditory person. But, but yeah, I felt like it was just very calm and relaxed and there was not a ton of formality, which I really enjoyed. And did you find that there was a learning curve to be a co-host of a room?
I, you know it initially, yes. I think the hardest part was just to figure out how to like accept the invitation and sign up quite honestly. And then after that, like, you know, it, it was, it was totally fine, but yeah, not more so than like. I guess Facebook or Instagram or whatnot and as direct pediatric care is growing as well in your area, if others wish to reach out to you after this podcast, what's the best way for others to connect.
Oh, for sure. Yeah, so they can text me on my business line 9 2 5 2 9 7 5 5 7 3, or they can email me and that's doctor@oliveleafpaeds.com. Wonderful. Thank you so much, Dr. Shree for joining us today. Thank you so much for having me. This was so fantastic.
*Transcript generated by AI, so please forgive errors.




Comments