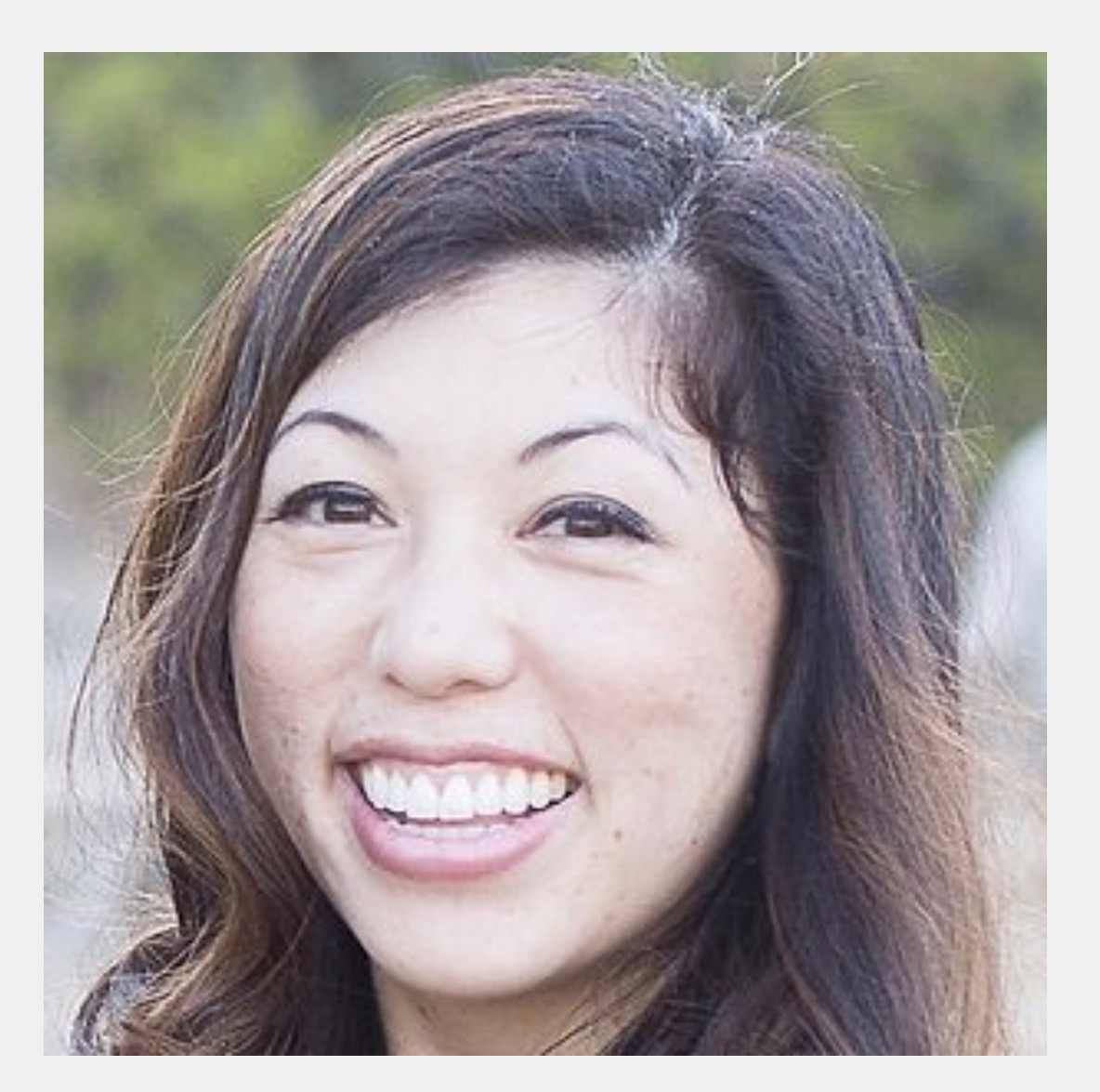
Episode 65: Dr. Nithya Natrajan (She/Her) of Blossoming Mamas - West Columbia, SC
- Maryal Concepcion
- Nov 21, 2021
- 41 min read
Direct Primary Care Doctor

Dr. Nithya Natrajan is a proud a mother of 3, a board certified Family Medicine physician, and Certified Lactation Counselor (CLC) with additional clinical experience and training in infertility, gynecologic care, lactation counseling, and breastfeeding medicine.
Her direct care practice, Blossoming Mamas, was born out of a passion for helping others transition to parenthood with personalized support using evidence-based medicine grounded in lived experience.
After dealing with infertility, pregnancy complications, birth trauma, and postpartum complications (including difficulty with lactation) herself, she shifted her focus to help others as they grow their families.
Her goal with Blossoming Mamas is to work with families to create positive pregnancy and postpartum experiences as her patient’s families grow with a special focus on the 4th trimester. To address this transitional time whilst families are adjusting, Dr. Natrajan eases the transition by offering telemedicine visits to assess lactation and coordinate care – physician to physician – with her patient’s personal OB and pediatrician and will also connect her patients with community resources as needed to ensure they get all the support and assistance they need.
She is proud to be caring for families in South Carolina and Georgia!
Dr. Nithya Natrajan joins us today to share about her practice where she pulls from her own experience as a Mama to help her patients in their fourth trimester journeys. Dr. Natrajan grew up watching her father practice medicine and deciding early on she was going to be accessible to her patients on her terms; in her all virtual practice, she is able to achieve just that.
Resources mentioned by Dr. Natrajan:
IABLE - Primary Care course and Certificate in Lactation Counselling - Jan 8 and 15, 2022
Doctors Practicing Breastfeeding Medicne, a FB Group
CONTACT:
IG: blossoming_mamas
Website: Blossomingmamas.com
TRANSCRIPT*
Direct care means that I'm able to take care of my patients the way that I want to. What that means is I'm able to listen to their stories, give them the evidence and help them make a personalized care plan that works for them. You know, in traditional medicine, so much of your time is spent doing administrative tasks by going to a direct care model, I'm able to refocus the relationship on myself and the patient so we can really make a plan that works for them. I'm Dr. Nithya Natrajan with Blossoming Mamas and this is my direct care story.
Welcome to the podcast. Dr. Natrajan thank you for having
me. You are, uh, another mama who has. Little ones under the age of five. And your youngest is now four months old, which is just crazy.
And you are also a direct care doctor. So it is, it's such an honor to talk with you. And I wanted to start with the fact that you are the daughter of a physician and you had been able to see. The world of medicine with the influence of insurance prior to opening your practice. So can you share what was your experience like at your dad's practice and what kind of doctor is.
So my,
my dad is, uh, he's trained in reproductive endocrinology and OB GYN. Currently he'd known her does surgery, so it's all office based practice and he focuses on non IVF, infertility hormone therapy. And then he does a lot of general GYN care because his patients just kind of keep coming back to him.
And so after I finished the fellowship, we had our first baby and I was not sure if I wanted to go back to clinical medicine. So I ended up going back to my dad's office and I practiced with him as a locums for about two years before our second child was born. And it just, it was just an amazing experience to see how he practices and how his office works.
So he does still take private insurance, but he does not take Medicare anymore. And he has a good bit of cash pay because of that. And so much of his time. I spent on that doctor patient relationship because he has a small enough practice that he can do that. And because it's a private practice, he kind of has control over how his schedule work and who stays work.
And so just, just seeing that, that still exists, I think made an, a really big impact on me to say, Yeah, I can still do this. I can still do patient care, but maybe do it in a way that works better because you know, and I think in most residencies and fellowships, it's all insurance based care. You have very short visits, you can't get to know your patients very well.
And all of that kind of made me feel like maybe I don't want to do medicine anymore. Where as looking at my dad's practice and seeing the type of relationships and practice he's built, I was able to see that there are other ways to do this.
It's so lovely to hear that you had that experience of training and also the other side of the fence. So to speak in that you're you saw your dad's practice.
What types of conversations did you guys have when you were mentally exploring the space of, I love what you're doing. I'm realizing that I can do this in my own way. I'm actually thinking about opening up my own practice. What were those conversations like in that transition period for you and your.
Well, so it was it's interesting because when we had our second child, I had actually decided to leave clinical medicine and I was planning to just do a non-clinical position that I've had at Medicaid. And just focus on that. And I did that for about six months to a year. Before I realized, you know, I, I really miss the patient care part of it.
And when I talked to my dad about it, he was like, I don't know, you know, in India, it's really hard to survive in this world if you don't take insurance, because that's kind of what a lot of patients want. And you know, the reason that I can do it is because I've built these relationships over 30 or 40 years.
So when he quit Medicare, he did have patients leave, but he still had a good portion of his patients that said they didn't care. They wanted. I see him. So they, they were willing to pay for it. But, you know, I think when I initially had that conversation with him, he was, he had never really heard of direct primary care.
He he'd heard of like concierge medicine and things like that, but he was kind of like, I don't know if he can really do a specialty, uh, and, and, you know, focus your practice like that. And also say you're not taking insurance. So initially he was kind of, you know, I think he gave me a re he was trying to give me a reality check and I was kind of like, I don't want to reality check, you know, it's either I need to do this my way, or I don't think I can do it at all with the way the insurance systems are set up these days.
And so, you know, I think for him initially, he was a little hesitant. And then as I started building things and talking to more people and learning about their practices, and I explained to him, you know, why I think this could work. He. Come on board. And I think now he's just, he's just excited and thrilled and happy to see that, you know, it is something that can be done and that there is a way to get out of the system that this kind of trapping positions and trapping patients and not really working anymore.
And you're doing it while taking a break for your own maternity leave with your latest little one and who is now four months old. So. That's awesome. And congratulations, you know, for, for doing this and making the jump and educating your dad, and I'm sure he's probably told other physicians about the fact that you're doing your own thing and it's in alignment with the way you want to do medicine.
Now, in addition to the conversations you were having with your dad, what were the mental plans that you were actively making before opening your practice in order to open the practice that you desired to? You know, I think
the first thing was just figuring out what I wanted to do with my practice. And I think in the fourth trimester space, which is what I focus on is, uh, is something that's really developing.
There's just not that many people doing it right now. And so it, it really was about defining what I'm able to do and what I want to do. Now versus what, you know, in five or 10 years where I'm hoping to be. And so I, since we have such little children and since we're in the middle of the pandemic, which is kind of a crazy time to start anything, you know, it just made sense to start it all virtually, both for protecting my family, but also to protect the families.
You know, these new infants, like just to help them get half an option where they can be seen from home. So I decided to really focus on that fourth trimester and then focus in on breastfeeding because we had a lot of difficulty with breastfeeding. I couldn't find any specialists locally. That was a physician that understood breastfeeding enough to help me with the problems that we had with our first child.
So that was why I decided to focus on that. And I knew that was what I wanted to do. And then I. I spoke with, uh, Dr. Rebecca Behrens, who I think you had on a while ago, she was kind enough to talk to me after I asked a question on the physician entrepreneur group and she is kind of the one that really got me started on like, Hey, I can do this.
I can make it a reality. And so that's when I started exploring all the logistics of how do you set up a practice and what are the different pieces that need to be in. To be able to open up. So that's kind of how it evolved is like I had this idea for, this is what I want to practice. This is how I want to practice.
And then I went from there to, this is how I make that happen.
Wonderful. And I love that that tie in it's if we all talk about. The word of mouth is the way to network about our practice. But I love hearing stories about the word of mouth, about DPC as a model is getting out to other physicians and inspiring other physicians to, to learn about the movement and to potentially jump in.
On your website. In addition to talking with your dad, you had also talked about having a conversation with your sister about your practice. And so I want to ask about that conversation because speaking with somebody who is a non-medical professional is sometimes very different than when we talk to a physician, especially who is understanding of the fee for service model.
Right. So with my sister, it's interesting because she was kind of the one that even pushed me to start thinking about, you know, providing the service to people.
She was really struggling with feeding her daughter. And the first time they came to visit her daughter was about two months old. And our second child was also about two months old because. They use within like two weeks of each other. And she came here and she was just always feeding her baby. And so we sat down and I asked her, you know, is it okay if I try to help you?
This was before I had done any training or anything. And it was like, she was uncomfortable. Her baby was uncomfortable and it didn't seem like she was getting any milk. So we talked through it and figured it out together. And you know, it, it was crazy because when she was leaving. My house is when she was like, you should do this for other people.
Like what, you know, you actually understand the medicine and you've breastfed your babies. Your, you know, your first baby, you went through a lot of struggles and it just makes sense for you to provide this as, as a service to other people, because you could really help them with your medical knowledge in addition to the lactation portion.
And I was kind of like, yeah, right. You know, I don't know. That's not, you know, how, how am I going to make that work? I have all these little kids at home and now. The focus on my nonclinical work and all of that. And she was like, I don't know Nythia but you need to figure it out. And so it was maybe like six months later when I talked to her Becca.
So it was like six months of just thinking and trying to figure out, you know, is there even a way that I can make this work that would make me happy. And then after talking to Rebecca, I talked to my sister again. I was like, Hey, I think I'm going to do this. That's awesome. Just let me know what I can do.
And I explained to her, you know, I don't, I don't think I can take insurance. Like I just can't do it and run, uh, you know, have a small practice. And she was like, I mean, I think it makes sense. I think this is a service people need. I think it's a service that very few people offer. And if you put it out there, I feel like moms are going to come to, to get that help because they just can't get it anywhere.
And you know, it just, I think that she was very accepting of it because she had gone through that and knew how. Pain and struggle. She went through and in a place where she couldn't find anyone to help her, like everyone was like, it's going to be fine. Just keep going. It's you know, and I think there's this tendency to do that to new moms, like just push through it.
It's going to be okay. And sometimes, no, it's not okay. You know, someone can help you. And that, that was kind of her whole reasoning. She was. You know, I think you should do this. And I think you can do this because it's a space where people need help and they're not able to find the help they need.
And for you, as you explained earlier, you have skin in the game in terms of you understand that it's not just, Hey, I gave birth to your baby.
And now the baby's eating no problem. As his fellow physicians, we've seen that it is not a hundred percent where a baby will go from being born to breastfeeding successfully. And as you're describing like you and your sister experienced challenges, when it came to.
Successful breastfeeding. And so when I look back into my own training, in terms of working with IBCLCs and the hospital, I loved the IBCLCs that I worked with . There are amazing people, but it's similar to when we choose to not do fee for service medicine. Had expressed the frustration when it comes to , not really having time with their patients and on the receiving end of that.
Having had both of my babies in a hospital, you know, even, even when you're medically trained, when you're flipping exhausted, because you've just delivered a baby and then somebody tells you when you're half awake, How to breastfeed in 20 minutes, maybe for two days in a row, that's a really steep learning curve to be on when you have a new little one to take care of, you're exhausted, possibly in pain.
And then having to remember to breastfeed
yeah. And I think even as positions, you know, I, we don't get any training in breastfeeding, really very minimal training in breastfeeding.
And, you know, I, I think IBCLCs are wonderful if they do a great job at what they do, but they're not, they're not trained to think medically. So then when there's a problem, right, they're not really trained to think through, this is the differential diagnosis. This is how I manage it. This is what could be going on hormonally.
This is what could be going on physically, right? I mean, they, they're wonderful, wonderful, wonderful. What they do, but their role is not to be a physician. And unfortunately, you know, the way that breastfeeding is in medicine and in our culture, a lot of the times it's kind of not really talked about or understood.
And so, you know, I think it's a space that is thankfully growing. I think more people are getting interested in this field. But there's just not that many people doing it right now. So I'm just, I'm glad that I'm able to offer that service and hopefully, you know, able to help, help moms meet their goals and figure out what's going to work best for their families.
Because at the end of the day, that's, what's most important is to find what works for them, not to force an agenda on it on people or make them do something, but figure out a way to. Set up something that makes them happy. Right. And with direct care, I'm able to do that because we actually have time to talk to people and understand what their needs are and then figure out how to meet those needs with evidence-based personalized care
and a relationship that doesn't have to happen in the 20 minutes.
You know, you're allotted in the hospital, but you can have multiple conversations with a family if needed. So I want to ask about your practice specifically. So can you share when a patient finds Boston mamas, what does it look like in terms of the type of services that you provide as a physician?
So I I've got a couple of different options.
So I do have a fourth trimester package, and this is a more comprehensive package. It's a $500 total, but it's like four months of care. And so what I typically recommend is in that last month of pregnancy that people meet with me so we can assess what their goals are, understand what they would like go over kind of, you know, what to expect and how to establish a breastfeeding relationship.
So that way they have that knowledge. Before they're in the hospital postpartum possibly, you know, still with medications on their system. And. Totally the world has totally changed with this event. Right. So it's hard to focus in that situation. So I try to meet with them beforehand so we can go over.
What does breastfeeding look like? What can we do to plan for your fourth trimester in general? What support systems can we set up? So. But what kind of a person has it in the package? And then after delivery, we do two more visits. So one is right after delivery to check in, make sure everything's going okay.
Assess for any problems. And then I have another visit where I kind of leave it up to them, what they want to do with that, if they want to do, how do I do a return to work schedule, or if they have a problem. And then I have reduced rates for any additional visits. And I also offer text messaging support from whenever they start in their pregnancy through that fourth trimester, which is the first three months after they deliver.
And so they they're able to get text messaging support through that, and then they get those three virtual visits with me and then discounts on anything else. Uh, if they don't want to purchase the package, then they can just purchase each of those visits individually. So if someone just wanted a prenatal visit to get an idea of what they needed to do to prepare, they can do that.
If someone just needs to be seen postpartum, because they're having a problem, we can do that. Or if they want to set up a visit to figure out how to return to work, then we can do that as well. But I'll usually set that. More as like that post full postpartum visit. So we have time to discuss everything.
So the, the way that my practice is set up, it's like, I'm trying to give people options because I know that, you know, motherhood is, and parenthood is transformative. And a lot of times people don't know what they need ahead of time. So for those that like to plan or want to plan, I have that option to get that package during pregnancy.
For those that may just need to be seen for an acute visit. I also do offer more of, I guess, like a fee for service, individual visit option as well. Now
you mentioned earlier that you opened as a telemedicine only practice. Are you still offering telemedicine visits exclusively or are you doing in-person?
So I'm currently still only offering telemedicine. And then I started with just South Carolina, but I'm licensed in Georgia as well. So I was able to set up to where now I can see patients located in South Carolina or in Georgia. And if you're not one of those states that want to fly in, I'm happy to see you.
As long as you're physically in the state. I can see you. I don't have any. In-person visits right now because we do have a young baby at home. We have young kids and with the current state of the pandemic, it just, it it's not, I don't, I don't th I don't feel like it's a good idea to start in-person visits right now.
My eventual goal is that I can add in home visits and I can hopefully eventually get a physical location as well as patients prefer that. But right now, it's all just worked well. And it's all for mom. So I will kind of help position baby and things like that. But if baby is having a problem, I do require that patients have a pediatrician or a family medicine physician that can coordinate with me on taking care of the baby, because it just, I mean, he would just can't provide good care on tele-medicine to young babies and young children, in my opinion, because so much of it is reliant on talking to the patient and understanding what they're feeling.
Babies can tell you. Right. So right now it's all virtual, all focused on mom is by patient. And then I do help with baby's positioning and latch and things like that. Awesome.
You had mentioned earlier that you work with the family, you work with mama to see what will work for them.
And one of the things that you have on your website, which I love is informed as best. And so this informed part, I want to ask about when you have moms, who are your patients and who have this relationship with you, what are some of the most common things that you hear that you are addressing in
your.
To me informed as best. And that's kind of how I approach patient care and how I approach my patients. Because I think that our, our role as physicians is not to control people or tell them what to do it's to give them the information and the evidence so that they can make a decision that works for them.
And so to me, informed as best means that. I'm giving them all the information. Here's the data on why breastfeeding is, you know, is the optimal nutrition for infants, right? But we also need to look at your family and your entire person and how your fourth trimester is going, how your life is going. And how everything else is to determine what the best thing is for you and your baby.
So at the end of the day, my goal is to give people the information that they need to work with me to create a feeding plan that works for them. And, you know, my, my focus really is on breastfeeding and. Like certified lactation counselor. And that's, that's a big portion of what I'm doing. But if that is, that ends up not being the right thing for that family, then I've got other resources we can go to, to help them figure out what's right for them.
So, you know, I think that at the end of the day, my goal is to inform families so that they can make the best decision for them. And again, I think, you know, I don't think this is possible in other other care models, because with direct care you have the time to do that. Right. You don't have the time to do that in a 15 minute visit.
Like it, my initial visit is 90 minutes. So I sit there and I learned everything I can about my patients. And then I give them all the information they need so that they can make an informed decision about how they want to make their family work and how they want to make that fourth trimester work for them so that they can enjoy their baby and enjoy their family.
Just
wonderful. This idea of creating a space where you are. Helping educate people and inform people so that they have the tools to make the decision that's best for them. I think that that, that respect of, of, of, uh, of a family being able to make that decision, I'm sure that that's also creating a word of mouth reputation for your practice.
And I'm sure that, you know, that's how you'll continue to get referrals. If, if that's not
already happening. So as far as building my practice and finding patients, a lot of them have been referred to me by IBCLCs because they, they have a medical issue that is not being addressed. And so I think right now, a lot of those referrals are coming from other lactation professionals.
I'm hoping over time that, you know, the word of mouth will spread it more between patients. Uh, you know, the one, the one thing that is a little bit challenging when you're providing specialty care, especially when it's kind of focused like this. You don't get as much of that longitudinal relationship as you get in a full, direct primary care model.
And so I think that is a little bit of a challenge as far as having patients spread this, my word of mouth, but I I'm hoping that, you know, this will have an impact and that families will benefit from it. And hopefully, you know, spread that information to other people that may be struggling and need the help.
Now,
another branch of your practice is. In addition to providing support for mamas and their breastfeeding journey, you also offer pregnancy loss and infertility support consultations. So that is definitely something that as a mom, who's miscarried herself. That is something. What does that support look like? Because , I'm just thinking in my mind here of how amazing that would be to have somebody who is a physician talk with you about. Loss from a medical perspective, so, so please share about that part of your
practice.
So I actually added these consultations in, after I had finished building up all of the pieces that go into starting a practice. I hadn't opened yet at the time, but it was during and fertility awareness month. And I was thinking through it, we've had three pregnancy losses ourselves. You know, there wasn't really anyone to talk to about what happened or what to expect or where, where to go next.
Right after all of that happened. And thankfully, you know, my dad being an REI, he had lots of. Places for us to go and talk to physicians that were knowledgeable and caring, um, to help us. But I think a lot of patients don't have that support and a lot of them are, you know, unsure of what is going to happen or what to expect or what their choices are some of the time.
And so my goal with that visit is really. To help people explore what they've already been through and then to help just guide them through their process of whatever is going to happen next. And so I think it's really meant to be a support for patients where they can get information from a medical provider and really focused on the emotional aspects of it.
And the, you know, the, the different parts of it that often are left out. Right. With infertility. I think a lot of times it becomes very clinical when you're actually going through treatments. And so you kind of lose that human aspect of it. And that's what I'm trying to bring back with that, with those consults is to say, Hey, you know, I know that this is a difficult thing that you're going through.
You know, there's a light at the end of the tunnel, and there are ways to grow your family. Even if you're not able to conceive yourself, there are lots of ways to grow your family and you have options. And just, just to really provide some more of a, more of a human perspective on the whole process for people while still having that medical knowledge and being able to answer.
Any questions they may have. So, because I'm not trained as an OB GYN, I don't provide medical counseling for infertility issues, but I'm, I'm really here more to help guide people and give them things that they can think about. And talk to them just about how, you know, how men work, how your periods work, what options you may want to discuss with your doctor, that kind of thing.
And just, just really just. Them understand what may be going on and help them get through that whole process.
And do you see patients joining your practice while they're in things like IVF treatment so that they have the clinical part when they go to the fee for service doctor, but then they have the time and the emotional support and the understanding and the discussion part with
you.
So that, that is my goal is that this really acts as an additional outlet for them to kind of talk through and understand their options with someone that's knowledgeable about the medical aspect of it. Uh, and then I D I did spend two years with my, with my dad after fellowship, where I got to learn about a lot of this and just really explored.
What patients go through and that kind of thing. So that is my hope that this kind of acts as an adjunct to the people service reproductive assistance that they they're getting through the traditional system. I have not had any infertility consult yet. I mean, we, we just, we haven't been open very long, but my hope is that I can help them with that journey.
And then. You know, if they're able to conceive and they want to, they want to breastfeed, or even if they don't, if they just need additional support, you know, I'm hoping that they'll, they'll choose to continue and that we can make sure that they have a great overall experience as they become parents
with the recent academy of breastfeeding medicine endorsement of using the term chest feeding.
I want to ask how do you address chest feeding and breastfeeding in your.
I know the ABM recently released a statement and I was talking about this with a couple of other people that do that work in the space and, you know, to, to me, like I'm going to do whatever makes my patients most comfortable and use whatever pronouns they want, whatever terminology makes them feel heard and seen and feel comfortable and happy with their experience, you know, but we were talking about it.
Breast is not technically a gendered term. Men can get breast cancer. Men do have breast tissue. Right. And so I think that I will always use chest beating if that's the patient's preference, but I do tend to say breastfeeding and I use the terminology breasts because in a medical sense to me, that is, you know, that is the medical term for this.
Right. And so I think I'm still trying to like, I guess formulate my thoughts on that whole space, as far as what should be used in like the literature versus how you address it on an individual patient level on the individual patient level, I'm always going to do what, what makes my patient comfortable?
Right? So if, if you're like gender nonconforming and you don't. You want to refer to just being awesome. If you're trans and you've had top surgery and now you want to try to induce lactation or, um, you've had a baby and you're hoping to just feed and you want to call it chest feeding. I will totally do that.
But at the same time, I'm just not sure. Like, and things like social media and the medical literature, like I just don't know what the right answer is for, you know, what should that terminology be and how, how should it be phrased? I guess
now you mentioned. You are in Georgia and you are in South Carolina in terms of your licenses, how are you going about marketing?
In that your practice is actively growing right now. I'm
just reopening again now. But what I've been doing is reaching out to local doulas and IBCLCs and other birth workers to let them know about my services, because that's where I've gotten a lot of money. Referrals from, and then I'm also on social media right now.
I've been trying to do like little campaigns. My goal with that, I mean, you know, I think to some extent it is marketing, but my goal with that is really education. Like I want people to have as much information as possible. So even if they don't have a consultation with me, I want them to be able to get to some of these resources and have a basic understanding of lactation knowledge, because a part of what I'm doing.
And the point of what I'm doing is I want people to understand what is physiologically and biologically normal. For breastfeeding and how to make yourself be successful at that. Because unfortunately there's just a lot of misinformation out there. And even things like, you know, baby friendly hospital has done a lot of great things, but it, like at first it leaves the word mother out of the whole thing, right?
Like there's a dyad, there's two people involved in that. And second, I think a lot of the people that are in those baby friendly hospitals still don't understand breastfeeding or how it works physiologically. So my whole goal. Is both marketing and education with our social media. So a lot of it has been outreach to community providers, and then I'm doing the social media portion.
I have done some outreach to physicians, but I think because of the traditional fee for structure model, I'm just not able to get to the physician right now. So it goes to the office manager who never replies. And so it just, unfortunately I'm not having as much success marketing to that group at this point.
I think once things settle down with the pandemic, I think go out more and hopefully talk to people and talk to offices. I'm hoping to get more education and more information about our practice out into the community. That way.
Awesome.
Now you have a four month old and you've recently finished your maternity leave to open up your practice again.
What was that experience like having opened your practice, pausing your practice, and then reopening within the early development of your practice.
So. I feel like the timing it's interesting. This timing has always been like a little bit crazy for me and it, you know, I feel like it always works out for the best at the end of the day.
So I started thinking about all of this in June of 2020, and I was hoping to open by the fall of 2020. Which was extremely, I think that was extremely ambitious because it just, it takes time to do things, to set up a practice, right. You have to set up the LLC, you have to look at, explore all your options, look at what all you need to put in place.
And all of that is going to take some time. So I actually ended up opening in January of 2021 is when I really started opening my schedule up to see patients. And then we kind of unexpectedly got pregnant as well. And you know, I was due in April of this year. And so. When I opened, it's like I knew I was going to have to go out on leave in three months.
So I just kind of did it in a way where I wouldn't take any new consults in a period, but you know, like I wouldn't have any active patients during my maternity leave, which I could do because it's a specialty practice. And then it was early enough that I didn't have many. People needing consults anyway.
So it ended up working out. And so now I'm kind of reopening and in some ways kind of restarting with a lot of the marketing and getting the word out there. Now that we're open again. But yeah, it's, it's just been interesting and, you know, I think it's, it's always, uh, You're always juggling a lot when you have young kids.
And so that's definitely a piece of it as well. Just making sure that I keep that balance for my kids and make things work for them. But the beauty of being your own boss is you can make decisions about that kind of thing. Right? You're like, Well, I don't have any patients on my schedule this Wednesday, and I need to hang out with the kids more.
So let's just block it and go to the zoo or like go to the beach or do something. Right. And you have that freedom as, as a direct care doctor to say, I need this time for myself. And then I'm going to work, you know, tomorrow evening to do whatever I was supposed to do today. And you can do that. And so it just, it's just a balancing act.
I think, uh, It's something always needs more attention at some point, right? Like it's never perfectly imbalanced, but you can kind of make it work, I guess. I love
that. And I'm biased because now I want to plan a zero day.
My DBC is amazing, you know,
with that said, what is your overhead like when you decided to be a telemedicine only practice for that?
So the overhead with telemedicine only, I was able to like really minimize costs. So, you know, I think at most it's been like, The initial startup was, was probably about three to 4,000 to get everything going and, um, you know, get everything in place that I needed in place. And I would say my annual overhead is really going to be mostly credit card processing and then maybe.
Four to $500 for some of the things that need to be maintained. And so it's this really low overhead costs. Um, oh, and sorry, it's going to be more than that because of malpractice. You may be like two to 3000 a year, but the majority of my overhead is in malpractice insurance right now. And then the other things that I paid for.
So I have to pay for our website ease and then, um, local business licensing fees. Uh, and then I have a PO box and then I have a registered agent because I run everything out of our house, but I don't have rent. I don't have anything else to really worry about right now. Um, and then, you know, like occasionally I'll have to purchase marketing materials and that kind of thing, but it's, it's really, really low overhead at this point.
Like the highest cost, like I said, is the malpractice insurance and the startup costs like. Setting up an LLC and that kind of thing. That's probably where most of the money went at the beginning. Um, but still malpractice was still the biggest portion of the startup at that point as well. So it's low overhead, you know, I think.
I think I have to see like 10 or 20 patients a year to cover my overhead. It's not that many patients. And so it just, you know, like it, it, it's not like it's not something that I have to worry about breaking the bank on, especially with the young kids. And if I don't get a ton of consults, it's not the end of the world because.
That my overhead is not that high. And then it's a tax deduction if I'm, you know, if I'm negative. So it's a tax deduction from my other job or from our, our other income. So I would say, I mean, it was a good way for us to start. It's something that worked well for our family. And then, you know, once I've kind of gotten.
Going and hopefully they'll pandemic is over. I can look at expanding it into more of a home visits and physical location and things where there's going to be more overhead at that point. And when
you talk about your, when you talk about income in part, uh, from blossoming mamas, and then in part by other things you touched on your Medicaid job.
So what does that look like for you and how did you come to find this Medicaid job?
Um, so my job had Medicaid. I, I worked with them to review applications, so it's all nonclinical. And I basically get a file with a patient's entire chart and I review it and then let them know, you know, how much work I think that person can do.
And then they make a determination on whether they think that person needs to go to a full-time job, or if they qualify for Medicaid. Um, the way that I found it is through one of my attendings from. Residency. So she used to be in this position when she had little kids, she used to be an attending and she did full spectrum family medicine as an attending.
And then after her babies were born, she did this Medicaid position for awhile. And she and I were talking, I was kind of like, you know, I'm not sure what I want to do. I don't want to sign on for a full, uh, full time. Position as a physician right now. Um, and she's like, I think that you would really like this.
It's a very flexible, it's great with little kids. Like, you know, it's, you're not seeing patients. So if an emergency comes up, you're not like leaving a patient hanging if you can't go in. And so I found it through my old residency and the med school I'm hired through the university's med school currently, and then like subcontracted to Medicaid, but it it's been really nice and it's a good way to have a steady.
But also, still have flexibility since it's not direct patient or it's not patient care and it it's, it's worked out well. But I think a lot of those non-clinical positions, it's people find in all kinds of random ways. Like it's not really like one specific place you can go to. There is a nonclinical career academy where people can learn more about some of these other side jobs, but, you know, I, I think it really was just kind of by chance that I found.
Awesome. And in terms of your ability to practice in glossy mamas, as well as continuing your Medicaid job, are you planning on the Medicaid job going on along with Boston mamas or do you see it transitioning more to only your own practice as the kids grow?
Um, so, you know, the, my plan right now is to continue to do both, actually really enjoy my work at Medicaid.
I feel like it's valuable. I feel like I'm able to help people and, you know, I do my best to help, help those out that really need it. So, you know, looking at it medically, like I really try to. Focused on what the patient needs. So I enjoyed doing the work that Medicaid, my plan is to continue working there probably, you know, about half the time and then do, do my practice the other half.
And right now I'm doing everything part-time with the baby. So I'm do I have about 10 hours a week toward blossoming mamas and then 10 hours a week, uh, toward Medicaid as is my current schedule.
So this next question is when. Coming from when I spoke with Dr. Whitney Pak, who, when she was in practice at Cortez, pediatrics was not able to see Medicaid patients.
So are there, I'm assuming there's no restrictions in South Carolina for you to take Medicaid patients as a direct care practice.
So currently, I, I decided not to see Medicare or Medicaid patients because I D I can't opt out of anything because of my position at the university. So my practice, my LLC does not take any Medicare or Medicaid patients because of that.
And then with private insurers, It's up to patients if they want to use their insurance or not. So there's not an issue with them and I can still give them superbills if they want it, because I'm out of network with everyone still. But because of my position at the university, I cannot opt out of anything.
So I can't can't see Medicaid or Medicare right now. You know, eventually I'm going to try to see if I can do like a scholarship set up for people that can't afford it, where, you know, they would be able to like apply for a scholarship and get free services. But that's not something that I have the capacity to do right now.
Gotcha.
Yeah. Thank you. Thank you for addressing that. Now, how did you decide on your tech that you use for your practice in terms of an EMR? And did you envision your EMR growing with you? When you decided to choose which one, whichever one you did.
Yeah. Um, so, you know, I think there are, there are so many options for EMR.
There's so many options for everything, right. It can get overwhelming. So what I ended up doing is I kind of tested out several different options. There's no way to test them all because there's just hundreds and hundreds. And, you know, my goal was to kind of do something that would have lower overhead because it it's something that this is kind of like.
It's my side gig. Now I'm hoping it'll grow into more of a full-time gig eventually. But with that, I ended up choosing a charm, which is free for up to 50 patients a month. And the way my schedule is because I'm quarter time. And because of the amount of time I spend with. I've never really going to be able to go over 50 patients a month.
Like I think I have 40 patients lots of month. So essentially my EMR is free right now. Is it perfect? No, but it's good. And it works. And a lot of birth workers use it, which is helpful as well. And it does have nice functionality and it's nice that I can just pay for the portions of it that I need to use.
So right now I just have to. Harm, and I can pay additional if I want to get a fax line through them or get e-prescribing through them. So it's, it's been working for me so far and, you know, there are other options out there that I looked at, like Athena takes a percentage of what you make, but you know, it doesn't make sense at all to.
Use Athena, if you're doing direct care, because a lot of what they do is insurance billing for your practice. And then of course there are several other ones, like Atlas I think, is really focused on like direct care model. So there's, there's just tons of different options out there. So I think those were like the three ones that I looked into the most, but then just to kind of manage overhead, knowing I would be on maternity leave and knowing that I wasn't going to have a lot of volume, I decided to choose charm.
And then if things grow or if I decide to go more into the direct primary care space with the sub practice of, you know, continuing with the port trimester stuff, I would likely switch to something that's a little bit more inclusive and robust. Right. I don't have to worry about adding pieces onto it, you know, kind of having everything together.
And one place. So for right now I chose charm just because of it being functionally, what I needed and being cost-effective for our prime.
When you're doing a micropractice solo doctor telemedicine clinic, it's definitely, like you said, it's a totally achievable, and I appreciate you for mentioning just the overhead costs that you experienced to give other people who might be interested in doing a telemedicine model or incorporating telemedicine, uh, as a, as a package, some inspiration there.
And I think that's great also that you are working with what works for your practice in this case term is free under the 50 patients per month. I mean, there's things like I prescribe, which is a free e-prescribing platform. And so, you know, there's definitely ways to. Make it work for you. And this is where I definitely would say talking with other direct care physicians like you did, Rebecca, it really helps because sometimes we don't know what, we don't know.
Like a Thena I did a walk through with them. And when other EMR is, and direct care are much more reasonably priced, I definitely felt that in addition to being focused on codes like that Athena in particular was very expensive. And for, for a practice. So finding out what works for your practice, I think is really, really smart.
And when you have EMR. You know, are being used in your community that I'm sure that helps. When you mentioned that charm is being used by other healthcare providers in your community, do you have portability, do you have easier portability with patients information because
of that? So with the patient charts, you know, it w what, the ones that I've had, I kind of create my own chart, but we can message back and forth really easily within charm.
And then there are birth workers on a couple of other platforms around here, but a lot of them are using charms. So it just makes like messaging back and forth and saying, Hey, can you see this patient really easy? Like if, if I need a baby that needs to be seen in person, and I really want them to see a lactation, right.
I can shoot a message over to like that ECLC that I know locally that does one visit and say, Hey, I have this mom and baby that really needed in person visit. Can you see them? And, you know, they can access and send whatever information I need through that messaging system. And it's all within the EMR.
So it's all secure. And so I think it does help to have that, but I think the biggest thing was it just made sense financially to go with charm and. It's easy for me to upload and then important data from my fax line, which I have a Doximity, which is also where, where I use my video visits. And so it just, it just is, I have a couple of different platforms, I guess, which so it's not totally integrated, but it's easy enough to go between them as needed.
So I think, I think that definitely is a plus that I can message them directly, but you know, if I was choosing. To have a more robust practice. I might choose something that's a little bit more inclusive, uh, as far as the features that it has, rather than that, just that messaging component.
With you being a physician who is able to have a practice revolving around breastfeeding medicine, as well as, pregnancy loss and infertility for other physicians who are wanting to educate about those areas of medicine. What resources would you recommend? They look into to expand their knowledge, to possibly expand their training before opening a practice that provides that type of.
Yeah. So, you know, there's several risk, there's a lot of resources out there for lactation training.
So the things that I'll tell you about what I did, and, and then I'll kind of summarize, you know, what options people would have. I ended up doing the certified lactation counseling training course, which is a five day course. That's really a basic education on breastfeeding and my patient. Okay. You know how normal lactation physiology works and it's not geared toward physicians, it's really geared toward anyone that wants to provide lactation support.
So I did that training and then, uh, I got more involved in various communities of breastfeeding medicine positions and people that are interested in doing breastfeeding medicine. So I learned about a couple of different conferences through there, but I would say one of the big. Educational sources for physicians.
Is I able, which is just, it's just a fantastic resource. I did their comprehensive conference last year, but they have a whole, whole array of options and they're comprehensive conferences. Great. I mean, it really went into like lactation physiology and what are the different problems and how to manage them?
What are our differentials? So it goes through kind of like, how do you think about lactation as a physician? But they also have four dark horses, like a primary care course. If you just want to incorporate this into your practice and kind of maybe help some moms out to the extent you can and then refer on.
If there's something beyond your scope, that's a really great option and they have monthly cases as well. And if you sign up for the. Uh, comprehensive conference, then you also get membership and I able, and so they all send out like research articles every week and they have all these great discussions on their listserv.
So that was just a really great educational resource to start thinking about lactation from a physician's perspective, the academy of breastfeeding medicine does do. The research conference each year, that's focused more on, you know, new topics or current research and, you know, there's a lot going on a lot that needs to be more learned.
And so that is kind of helpful, but I would say, you know, if there's one thing you're going to do to learn about breastfeeding and you don't know that much about it, I would say the ABL is the best option for a physician just to get gain a baby. Understanding. And then, you know, I think a lot of what a lot of people do is just do this in their practice.
So like if your pediatrician or your family physician. You learn what you can and then you kind of are on the ground, figuring out how to help families. I found the CLC course extremely helpful just for a basic understanding. There are a lot of other courses out there and for people that are going for an IB CLC, you know, you need a certain amount of lactation education and a certain amount of clinical hours seeing dyads.
So there are things I think the lactation education resource, which is being revamped now. So the, I think LER is. It has not been positioned focus. It has had some information that is not necessarily medically sound in the past, from what I've heard from people, I haven't actually done it, so I can't speak to it much, but I've, I've heard that they're revamping it to create more of a physician ed level education course there as well.
But as far as what's out there currently, I think I. The best place to learn at a physician level of knowledge about lactation. And then, you know, things like the CLC course, if you just need a basic understanding, those are really helpful as well. And then there's a doctors practicing breastfeeding medicine group on Facebook.
And that's kind of where I learned a lot about these different resources and they have tons of discussions about this. I'm still trying to decide if I want to pursue the IBCLC. Or not, because again, to me it's all about function. Like what, what can I do to help people? Right. And I, I think that getting it would just be adding letters to my name.
I'm not sure how much additional practical. It's going to give, I've done all the education hours toward it. I just need patient care hours and need to take the test. But, you know, it's, it's just another certification to keep up with that. So, yeah. So I think there are a lot of resources out there that people can look into and that Facebook group is really helpful because it has a lot of the leaders in the field, in the group.
And so they can, they can kind of speak to different ways to make it happen.
Now I know that you talked about social media and your marketing. So I want to end with, could you share with the listeners five amazing things about breastfeeding that you love sharing with all of your patients?
Whenever you get the chance?
Yeah, I would love to that's that's a really great question. So, you know, the, I guess the five things I love to talk to patients about, so one of them is skin to skin care. Like this is, this is the, one of the things that I love about breastfeeding, I think is so, so cool. So if you put baby on mom's chest after delivery and you just leave the baby alone, can I say that again for the physicians?
Leave the baby alone. All of you, healthcare providers, just leave that baby alone. So if the baby is fine and stable, when they come out and they have good, AFCARS just leave baby on mom's chest, baby. We'll explore and we'll latch on themselves. You don't have to do anything. Mom does not need to do anything that baby knows what to do.
When they're where they're supposed to be, which is what their mom, right. And this is, this is not when baby is sick or, you know, mom is crashing or something. This is, if baby comes out and is healthy and mom is relatively stable, just that baby on mom's chest. And they will figure out how to latch themselves.
And it's just, it's just so amazing that, you know, these, this little creature comes into the world and they can just, they like sit on mom's chest and they can just smell where that milk is and they push themselves over there. And just latch on and have that first feed. And that can, that can just. So much, like it helps create that bond with mom and baby.
It helps not come in and helps make sure your hormones are boosted. And then they're like sitting there kicking your uterus. So it like helps make sure your uterus is climbed down. It's just amazing. And it does so much more than just breastfeeding. Right? It's just, it's about that bonding experience between mom and baby.
So that, that is one of my favorite backs is skin to skin immediately after delivery does so much. And if you would just leave mom and baby alone. They will figure it out. Okay. So that that's, that's probably my favorite lactation fact. So the second thing, when you're in the hospital, do your best to room in with baby, keep them near you and respond to their cues.
You know, take the clock off the wall, stop looking at your watch. Just feed them when they tell you they want to be fed. And if you look at our social media, I have a chart on like feeding cues and how to recognize when baby is hungry. And so if you just look at your baby and bond with them and figure it out when they want to eat and get them on.
A lot of times that is all you need to make sure you're getting enough stimulation to get milk in. You know, I think a lot of people say, oh, babies are supposed to feed every two to three hours. No babies are supposed to be at least every three hours, but I promise you, there are going to be times your baby is going to be like looking for that boob every hour, every 30 minutes, that is normal.
They are trying to make your milk come in. So just respond to your baby, put them on. When you know, they asked to be fed and try to keep them with. And interestingly, you know, when I looked at the studies moms that kept their babies in the room did not sleep any less. Then moms that had their babies in the nursery, but they had less stress.
They felt more emotionally connected and they just felt better overall. Now that, you know, there are certainly clinical situations where baby might have to go to the nursery, you know, either for you or for the baby safety. And if that's the case, that's fine. Or if that's your preference that you want them to go to the next.
That's fine, but just know that like keeping them there and watching them is a great way to help make sure that milk comes in and then. So the milk doesn't really come in. It transitions. There's always something there. The claustrum is there. It's just very small volumes, which is normal and fine. And you know, human babies have evolved to the point where they that's what they need for the first few days.
And then. You know, first three to five days, your milk will transition. It will kind of come in and that's also totally normal. So just give it a little bit of time. Keep baby at the breast, get, get them feeding as much as possible and follow up with your pediatrician. That way they can make sure the weight is doing well.
If there's weight problems or something else going on, it's important to identify that early. So let's see. So skin to skin, keep baby with you, feed them off in, wait for your milk. You know, it's, it's going to take a few days to come back. And then my last thing is, if there's a problem, please ask for help.
And if somebody is not giving you help. Find that person that can help you and is knowledgeable and understands and is going to be there to support you. Because the worst thing that I can think of, and I went through this myself, is to have this baby and really want to breastfeed and not have any support or have people telling you the wrong thing.
And unfortunately that happens way too often. And you know, I think maternal. Health maternal mental health, maternal needs are something that have been overlooked in our society for a long time. So if you need help, if you know, if you're in a lot of pain, if you feel like your baby's not transferring enough, if baby's not gaining weight, well look for help.
And if people are not helping you didn't find somebody that will because we're out there and I'm, you know, I'm always happy to help out if I can. And even if you're not in a state that I practice in, I will find someone to help you because I feel like. So important that we support new moms and new babies to make sure that they're both healthy and happy.
And that that at the end of the day is what my practice is all about is to help you understand breastfeeding, to help you understand how it works and to help you meet your goals. If that's something that you choose to do amazing.
And for those of, for those of the listeners who wish to reach out to you after this podcast, what's the best way to get a hold of you.
So probably the fastest way is reach out to me on social media. So you can find our social media on our website, which is www dot blossoming. Mama's doc. And if you go on there on my front page, there are links to our Facebook and our Instagram. And so you can message me through those. You can also, uh, directly book a consultation on through our website.
You just put your information in and pick a time on there, and then you'll be on my schedule. You know, if you have questions, if you need anything, I would encourage you to reach out through social media and then we can always arrange a phone call as well. You know, I'm, I'm happy to do a free phone call to just talk through our services, talk through your needs and, and see if that's something that will work.
And then of course, if you don't see a time that works for you. Reach out because I will make it work and make sure you get seen quickly because you know, if you're in pain or if there's a problem, I don't want you waiting a week or even three days or five days, I will make it work for you. So I'll find a way to get you seen as soon, as soon as possible to reach out to me.
Awesome.
Thank you so much for joining us today.
Thank you for having me.
*Transcript generated by AI, so please forgive errors.




Comments